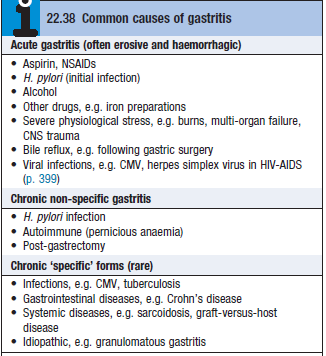
Acute gastritis
- Erosive and haemorrhagic
- Neutrophils are the predominant inflam cell in the superficial epithelium
- Etiology – MC from NSAIDs (see box)
- Clinical features
- Can often be asymptomatic
- Dyspepsia, anorexia, nausea, vomiting, hematemesis, melena
- Most cases resolve quickly
- Endoscopic biopsy – to exclude peptic ulcer disease or cancer
- Treatment – directed at underlying cause
- Short term symptomatic treatment with antacids, PPIs, prokinetics (domperidone), antiemetics (metoclopramide)
Chronic gastritis due to H.pylori infection (Type B)
- MCC of chronic gastritis
- Lymphocytes and plasma cells are the predominant inflam cells
- Correlation between symptoms and endoscopic findings are poor
- Most patients are asymptomatic and don’t require treatment
- Pts with dyspepsia may benefit from H.pylori eradication
Autoimmune gastritis (Type A)
- Involves the body of the stomach – spares the antrum
- Due to autoimmune damage to parietal cells
- Histology – diffuse chronic inflam, atrophy + loss of fundic glands, intestinal metaplasia, hyperplasia of enterochromaffin like cells (ECL)
- Circulating Abs to parietal cells and IF may be present
- Severe gastric atrophy and loss of IF lead to pernicious anaemia
- Some pts have evidence of other organ-specific autoimmune disease – like thyroid disease
- 2-3 fold increase in risk of gastric cancer in the long term
Drugs
Anti-emetics/prokinetics
- Metoclopramide [10mg/8hrs]
- Domperidone [60mg/12hrs]
- Cyclizine [50mg/8hrs]
- Ondansetron [4mg/8hrs]
PPI
- Lansoprazole [30mg/12hrs]
- Omeprazole [20mg/12hrs]
Antibioticcs
- Amoxicillin [1g/day]
- Clarithromycin [250mg]
- Metronidazole [400mg]
