- Severe inflam of the pancreas that begins like aseptic inflam but has secondary septic complications
- Mild parenchymal oedema →severe haemorrhagic pancreatitis →gangrene and necrosis
- CF – abdominal discomfort; severe illness with hypotension, sepsis, Multiple organ failure, metabolic derangements, fluid sequestration; death
Causes (I GET SMASHED)
|
|
|
|
|
|
|
|
|
|
|
|
|
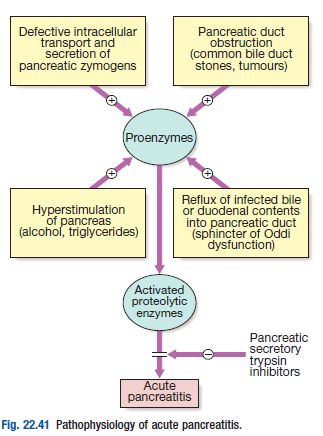
Pathophysiology
- AP occurs as a consequence of premature intracellular trypsinogen activation, releasing proteases which digest the pancreas and surrounding tissues
- Triggers – alcohol, gallstones, pancreatic duct obstruction
- Simultaneous activation of NFκB – leads to mitochondrial dysfunction, autophagy and a vigorous inflam response
- Severity of AP is dependent upon the balance between the activity of released proteolytic enzymes and anti-proteolytic factors (pancreatic trypsin inhibitor protein and circulating β2-macroglobulin, α1-antitrypsin and C1-esterase inhibitors)
Clinical features
- Abdominal pain – epigastric, radiates to back due to plexus and nerves (relieved by leaning forward)
- N + V. Decreased peristalsis
- Hypotension, hypoperfusion, depression – can be without Acute abdomen
- Turner (L.flank), Cullen’s (periumbilical) – severe acute hemorrhagic pancreatitis
- Pseudocysts – collection of fluid and debris in the lesser sac following and inflam rupture of pancreatic duct
- Initially contained in a poorly defined fragile wall of granulation tissue, over 6 weeks matures to form a fibrous capsule
- Pancreatic ascites – when fluid leaks from a disrupted pancreas duct into the peritoneal cavity
 Investigations
Investigations
|
|
Management
- Opiate analgesics – pain (pethidine [75mg])
- Saline/crystalloids – correct hypovolemia
- Catheter – shock
- Oxygen – hypoxic pts, and those with systemic inflammatory response syndrome (SIRS)
- Insulin – hyperglycemia
- Nutritional support
- LMWH – prophylaxis of thromboembolism
- BS IV ABs (imipenem, cefuroxime) – prevent infection
- Urgent ERCP – patients who present with cholangitis or jaundice in associated with AP
Complication
Abscess, fistula, bleeding, thrombosis, pseudocyst, peritonitis, shock
DDx
AMI, peritonitis, acute cholecystitis, ectopic pregnancy, renal failure, acute abdomen
Severity assessment criteria
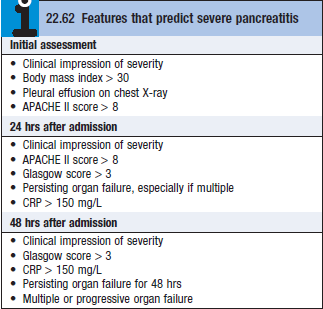 APACHE II, Glasgow and Ranson are all used. Please be mindful prognostic parameters are different for gallstone and alcohol induced pancreatitis.
APACHE II, Glasgow and Ranson are all used. Please be mindful prognostic parameters are different for gallstone and alcohol induced pancreatitis.
