- Severe inflammation of the pancreas
- Initially it is aseptic inflammation, but later has secondary septic complications
- Disease course – mild parenchymal edema → severe hemorrhagic pancreatitis → gangrene and necrosis
Etiology
- Alcohol – most common in men
- Trauma – most common in children
- Familial
- Biliary tract disease
- Iatrogenic – ERCP, operative, CT contrast, CABG
- Tumour
- Hyperlipidemia
- Drugs – azathioprine, OCP, furosemide
Pathogenesis
- Biliary stones/tumour – leads to obstruction of pancreatic duct, causing ductal hypertension
- Alcohol intake – leads to several consequences
- Hypersecretion of gastric acid and pancreatic juice
- Free radicals cause injury
- Spasm of sphincter of Oddi
- Activation of trypsinogen into trypsin → activates proelastase to elastase → activates prolipase to lipase
- Autodigestion of pancreas and necrosis of exocrine cells
Classification
- Pancreatic edema
- Destructive, necrotic form
- Local inflammation and complications
- Systemic complications, sepsis, multiple organ dysfunction (kidneys, liver, lungs)
- Fulminant form – kidney and liver insufficiency within 24 hours; death within 72 hours
Clinical Features
- Abdominal pain – epigastric, radiates to back due to plexus and nerves (relieved by leaning forward)
- Nausea and vomiting, fever, tachycardia
- Retroperitoneal haemorrhage
- Grey Turner’s sign – bruising of the flanks
- Cullen’s sign – periumbilical bruising
- Decreased peristalsis
- Severe attack – hypotension, hypoperfusion, hypovolemia
- Can occur in the absence of Acute abdomen
- Extra-abdominal manifestations
- Left pleural effusion
- Acute pulmonary failure
- Subcutaneous fat necrosis
- Cerebral insufficiency
Investigations
- Blood
- 3 fold increase in amylase
- Haemoconcentration – increased hematocrit and Hb
- Hyperglycemia – post-pancreatic diabetes
- Hypocalcemia, azotemia, abnormal LFTs
- XR, CT, US, MRI
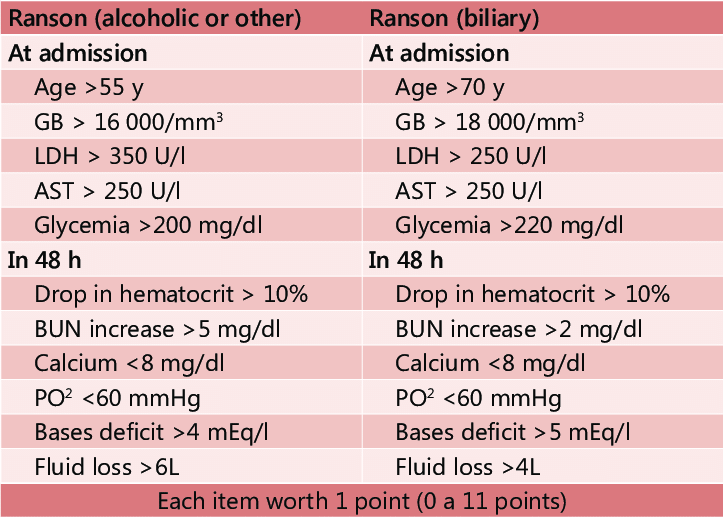
- Ranson’s Prognostic Criteria (see pic)
- Clinical prediction rule for predicting the prognosis and mortality risk of acute pancreatitis
Treatment
Non operative – Mnemonic PANCREAS
- Pain relief, Protease inhibitors
- Antibiotics, Anticholinergics
- Nasogastric aspiration
- Calcium gluconate
- Rehydration, Ranitidine
- Endotracheal intubation, Electrolyte management
- Antacids
- Swan-Ganz catheter for CVP, Somatostatin analogue (octreotide)
Operative treatment
- Open surgery is the gold standard for infected pancreatic necrosis – laparotomy and necrosectomy
- Indications
- Septic complications – abscess, cyst, necrosis, fever
- Organ failure – kidney, liver
- Biliary form of acute pancreatitis
- Fulminant form of acute pancreatitis
Differential diagnosis of hyperamylasemia
- Trauma, burns, abscess
- Carcinoma
- Biliary tract disease, intestinal obstruction, perforated peptic ulcer
- Salivary gland disorder, mumps, renal failure, diabetic ketoacidosis
