- Accumulation of free fluid in the peritoneal cavity
- Large volume (>1L) causes symptoms e.g. – abdominal distension, fullness in flanks, shifting dullness, fluid thrill
- Other symptoms – eversion of umbilicus, hernia, abdominal striae, scrotal oedema
- Dilated superficial abdominal veins if ascites is due to portal hypertension (PHTN)
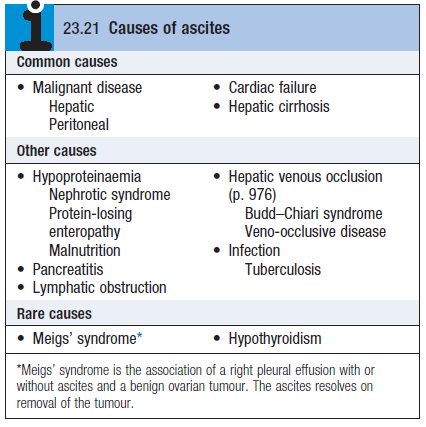
- Causes – see table
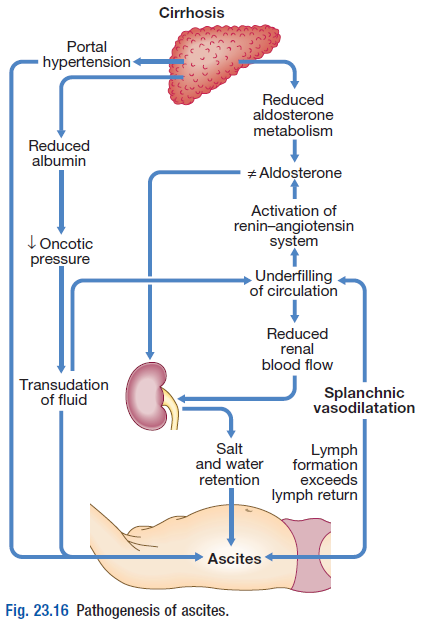
Pathophysiology
- MCC is malignant disease, cirrhosis, heart failure
- Splanchnic vasodilation – MCC of ascites in cirrhosis
- Mediated by NO released when PHTN causes shunting of blood into systemic circ
- Systemic arterial pressure falls due to splanchnic VD as cirrhosis advances
- This leads to activation of RAS with 2o aldosteronism, increases SNS activity, altered kallikrein-kinin system
- This system normalises arterial pressure but produces salt and water retention
 The combo of splanchnic arterial vasodilation and Pulmonary HTN alters intestinal capillary permeability – promotes accumulation of fluid in the peritoneum
The combo of splanchnic arterial vasodilation and Pulmonary HTN alters intestinal capillary permeability – promotes accumulation of fluid in the peritoneum
Investigations
- USS – can detect small volumes in obese pts
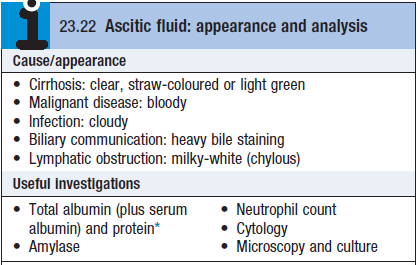
- Paracentesis – for analysis (see box)
- Pleural effusions on right ride – hepatic hydrothorax (CXR)
- Total protein content (TPC)
- TPC <25g/L – transudate
- TPC >25g/L – exudate
-
- Serum-ascites albumin gradient (SAAG) – to determine cause of ascites
- SAAG = serum [ALBUMIN] – ascite fluid [ALBUMIN]
- SAAG >11g/L – indicates ascites from Portal HTN
- SAAG <11g/L – indicates ascites from non-liver disease (neoplaisa, TB, Nephrotic syndrome )
- Amylase >1000U/L – indicates pancreatic ascites
- Low glucose – malignancy/TB
- PMNL > 250X106 – infection (indicates spontaneous bacterial peritonitis)
Management
- Transudate ascites – sodium and water restriction; diuretics (no more than 1L/d); paracentesis
- Exudative ascites due to malignancy – paracentesis; fluid management not required
 Patient should be weighted regularly
Patient should be weighted regularly- Sodium and water restriction
- 100mmol/d restriction
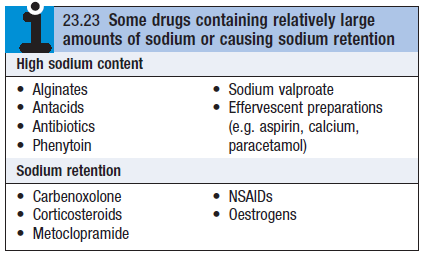
- Avoid sodium promoting drugs (see box)
- Restriction of water to 1-1.5L/d if plasma sodium <125mmol/l
- Diuretics
- Spironolactone (100-400mg/d) – powerful aldosterone antag
- SE – gynecomastia, hyperkalemia (must monitor)
- Furosemide – second line
- Spironolactone (100-400mg/d) – powerful aldosterone antag
- Paracentesis – first line tx for refractory ascites
- TIPS – relieves resistant ascites but doesn’t prolong life
Complications
- Renal failure
- Hepatorenal syndrome (HRS) – occurs in 10% of pts with advanced cirrhosis complicated by ascites. Mediated by renal vasoconstriction due to underfilling of arterial circulation
- Type 1 HRS – progressive oliguria, rapid rise of serum creatinine, poor prognosis
- Treatment – albumin infusions combined with terlipressin
- Consider pts for liver transplantation
- Type 2 HRS – in patients with refractory ascites; moderate and stable increase in serum creatinine
- Better prognosis
- Type 1 HRS – progressive oliguria, rapid rise of serum creatinine, poor prognosis
- Spontaneous bacterial peritonitis
- Abdominal pain, rebound tenderness, absent bowel sounds, fever – in pt with cirrhosis and ascites
- Can also present with hepatic encephalopathy
- Paracentesis – cloudy fluid, neutrophil >250×106
- MC organism is E.coli
- Treatment – broad spec antibiotics (cefotaxime or piperacillin/tazobactam)
