- Mortality is high – increases with age and associated systemic disease
- Precipitating factors – NSAIDs, H.pylori infection, coagulopathy, anticoagulation drugs
1. ANATOMY
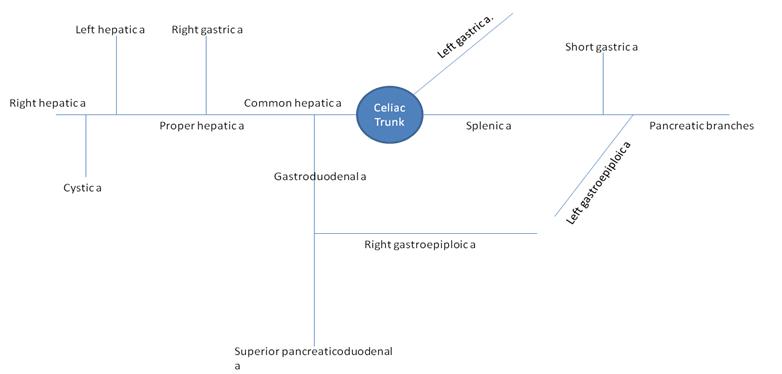
Branches of the celiac trunk
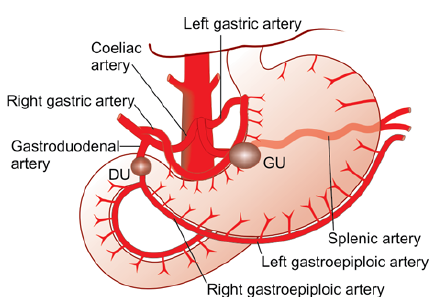
Sites of gastric and duodenal ulcer bleeding
2. BLEEDING DUODENAL ULCER
- Risk of bleeding in chronic duodenal ulcer increases if patient hasn’t taken anti-H.pylori therapy and PPIs
- A posterior ulcer is more likely to bleed
- Sources of bleeding
- Small vessels in the ulcer wall – less severe
- Erosion into the gastroduodenal artery – severe bleeding, needs early surgical intervention
Classification – Forrest Classification
Type I – active haemorrhage
- Type Ia – spurting and bleeding
- Type Ib – oozing
Type II – signs of recent haemorrhage
- Type IIa – visible vessel
- Type IIb – nonbleeding ulcer with clot overlying
- Type IIc – ulcer with haematin base
Type III – no signs of haemorrhage
- Type III – clean base ulcer (no clot, no vessel)
Clinical features
- Haematemesis and melaena
- Shock – pallor, tachycardia, sweating, hypotension, dry tongue, cold peripheries
- History of pain and tenderness in epigastric region which has recently increased in intensity
Investigations
- Gastroscopy is confirmative
- Flat clear based ulcer is less likely to rebleed
- Active ulcer/fresh clot/large ulcer are more likely to rebleed
- Celiac angiogram
- Hb% and hematocrit
- Blood group and cross matching
- Serum electrolyes, blood urea, serum creatinine, platelet count
Treatment
- Correct the shock – foot end elevation, IV fluids, CVP line, sedation, catheterisation, blood transfusion
- Stomach wash – adrenaline in saline through nasogastric tube
- IV ranitidine (H2 antagonist)
- IV pantoprazole (PPI)
- Endoscopic cauterisation of small vessels
- Sclerotherapy – with ethanolamine oleate or distilled water
- Cause tamponade, vasoconstriction and sclerosis to control the bleeding
Surgery
- Bleeding site is identified during laparotomy
- Under-running of the ulcer base with sutures and ligation of the gastroduodenal artery
Further treatment
- During discharge patients are advised to take anti-H.pylori triple therapy (omeprazole, clarithromycin, amoxicillin)
- Healing can be confirmed by gastroscopy after 6-12 wks
2. BLEEDING GASTRIC ULCER
- Similar to duodenal ulcer bleeding
- Severe bleeding is due to erosion into the left gastric artery
- Bleeding more severe than in DU
- Commonly present with severe hematemesis and shock
- Surgery is the main treatment
- Under-running of the ulcer base
- Partial gastrectomy with Billroth I anastomosis (gastroduodenostomy)
