- Neoplams of colon + rectum – hereditary, sporadic, familial
Etiology
- Diet – red meat, low fibre
- Alcohol/smoking
- Family history
- Previous cancer
- Neoplastic polyps
- Inflammatory bowel disease
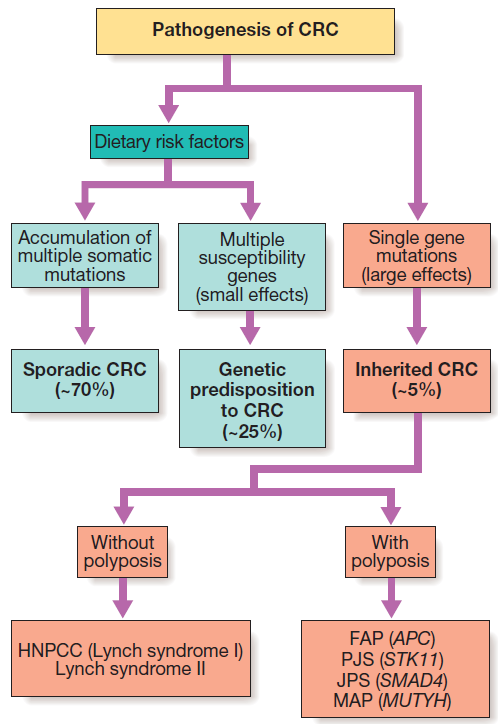
- Familial – FAP
- Hereditary – HNPCC (AD)
Pathogenesis
- APC gene is a tumour suppressor gene – on Chromosome 5q
- mutations can initiate the accumulation of genetic damage
- Colorectal polyps
- Any mass that projects into the colon lumen
- Can be sessile or pedunculated
- Removed via colonoscopy
- Peutz Jegher’s syn – AD
- Harmatomatous polyps + hyperpigmentation of buccal mucosa, lips, digits
- Polyps may cause bleeding or obstruction
- HNPCC – no polyps, AD
- Amsterdam criteria – 3 family members with colon cancer; colorectal cancer in 2 generations; 1 affected family member <50 y/o; FAP excluded
Pathophysiology
- Results from the accumulation of multiple genetic mutations arising from 2 major pathways
Chromosomal instability
- Mutations or deletions of portions of chromosomes arise, with LOH and inactivation of specific TSGs
Microsatellite instability (development of HNPCC)
- Germline mutations in encoding enzymes involved in repairing errors that occur normally during DNA replication
- Replication errors accumulate and can be detected in microsatellites of repetitive DNA sequences
- Result in genetically unstable phenotypes and accumulations of multiple mutations – eventually lead to cancer
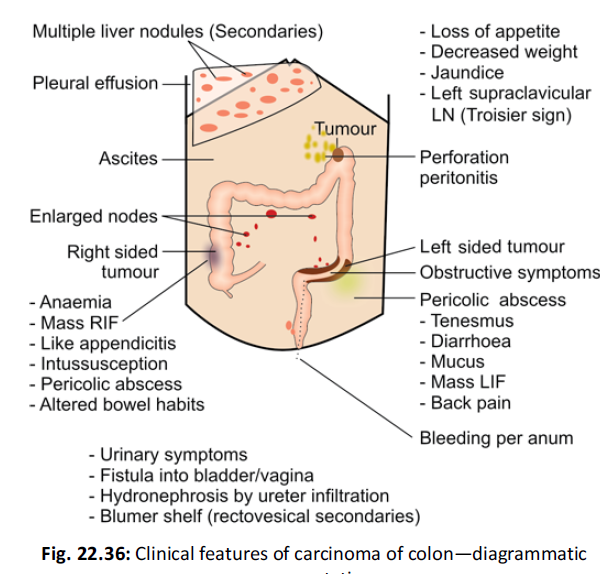
Clinical features – see diagram
- Left colon – fresh rectal bleeding and obstruction
- Right colon – anemia from occult bleeding, altered bowel habit, obstruction is a late feature
- Rectum – bleeding, mucus and change in bowel habit, rectal pain
- Other – pain, mass, weight loss, vomiting
Investigations
- FBC – anaemia
- Faecal occult blood
- Colonoscopy, sigmoidoscopy
- Barium enema , CT, MRI
- CEA – levels also increase in pancreas, gastric, lung, breast carcinoma; BPH
- CA 19-9,alpha-FP
- TRUS
Spread
- Local – bladder, ureter (hydronephrosis). Peritonitis or abscess
- Blood – MC to liver via portal v. Rarely spreads to bone, lungs, skin
- Lymph – pericolic, epicolic LNs
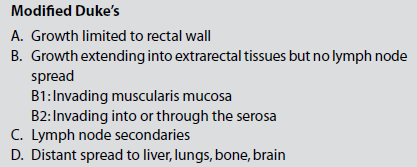
Staging – Modified Duke’s criteria
Medical treatment (for Duke C)
- FOLFOX regime
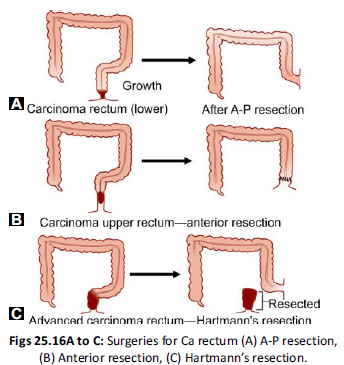
Surgical treatment
- Right/Left hemicolectomy
- Sigmoid colectomy
- Anterior resection – low sigmoid or high rectal tumours
- Abdomino-perineal resection – Miles, Gabriel, Lloyd Davis Operations
- For rectal carcinoma
- Removal of anus, rectum, part of sigmoid colon, assoc LNs
- Remaining part of the sigmoid brought out permanently – colostomy
- Proctosigmoidectomy – HARTMANNS OP
- For emergency bowel obstruction/perforation
- Resection of recto-sigmoid colon with closure of anorectal stump
- Endoscopic stenting/ Radiotherapy – palliative therapy