Etiology
- Alcohol – stimulates exocrine secretion, causes spasm of Ampulla of Vater
- Hyperparathyroidism – causes hypercalcemia, stimulates exocrine secretion
- Predisposes to precipitation of protein aggregates within the main pancreatic ductal system
- Congenital anomalies of pancreatic duct – pancreatic divisium
- Pancreatic trauma
- Developing countries – tropical pancreatitis due to nutritional deficiencies
Pathogenesis
- Hypersectretion and stimulation of exocrine pancreas and plugging of pancreatic duct with protein precipitates
- Leads to hypertension in ductal systems
- First attack occurs at the head of pancreas; second attack occurs at the body and tail (where the beta cells are)
- Hence, type 1 diabetes occurs after recurrent attacks of abdominal pain
Clinical features
- Patient has a history of alcohol abuse
- Epigastric pain – radiates to the back
- Type A pain – recurrent episodes of pain that resolve between attacks
- Type B pain – prolonged, severe, unrelenting pain
- Clinical tetrad – Abdominal pain, anorexia, type 1 diabetes mellitus, steatorrhea
- Peripheral neuropathy – related to diabetes
Diagnosis
- XR – pancreatic calcifications
- CT – golden standard
- Shows pancreatic calcification, dilated major pancreatic duct, pseudocyst formation
- Endoscopic reterograde pancreatography (ERCP) – protein precipitates, ductal dilation
- Pancreatic function test – Lundh’s test
- Meal of protein, carbohydrates, fats injected into stomach
- Sample of duodenal juice taken and activity of trypsin measured
- Positive test – low trypsin activity means decreased exocrine function of the pancreas
Treatment
Non operative
- 3 areas to manage
- Control of abdominal pain
- Treatment of endocrine insufficiency
- Treatment of exocrine insufficiency
- Abstinence of alcohol
- Small volume, frequent, low fat meals
- Pancreatic enzyme supplements
- Octreotide (somatostatin analogue) – decreases pancreatic secretions
- Exogenous insulin therapy
Operative
- Endoscopic pancreatic duct stent – to decrease pressure in ductal system
- Puestow’s operation (pancreaticojejunostomy) – to allow drainage of the duct
- Not recommended as intestinal bacteria can enter the pancreas
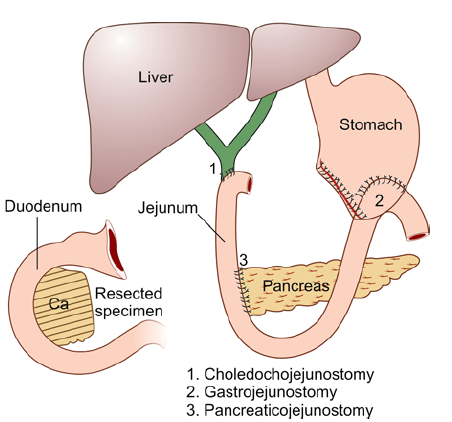
- Whipple’s operation (see pic) – pancreaticoduodenectomy
- 3 anastomoses – pancreaticojejunostomy, choledojejunostomy, gastrojejunostomy
Complications
External pancreatic fistula
- Drain tract left in for >7 days is a predisposing factor
- Classification
- Low output fistula – <200ml/day
- High output fistula – >200ml/day
- Complications – sepsis, fluid and electrolyte imbalance, skin excoriation
- Diagnosis – laboratory exam of fistula shows increase amylase, trypsin, lipase
- Treatment – parenteral protein; no oral intake of food; octreotide to stop exocrine secretion
Internal pancreatic fistula (pseudocyst)
- Localised collection of pancreatic secretion in a cystic structure – lacks epithelial lining
- Can cause haemorrhage
- Clinical features – abdominal pain; early satiety, nausea and vomiting secondary to gastroduodenal obstruction from mass effect of cyst
- Diagnosis – increased amylase, CT (gold standard)
- Treatment – internal drainage. Roux-en-Y
Pancreatic ascites and pleural effusion
- Due to pancreatic duct disruption, leads to leakage and collection of pancreatic secretions in the peritoneum
- Alcohol abuse is the most common cause
- Clinical features – painless massive ascites
- Diagnosis – paracentesis shows increase amylase and albumin
- Treatment – stop oral intake; nasogastric suction; paracentesis; octreotide
- Thoracocentesis for hemothorax or empyema – midclavicular line 2nd and 5th intercostal space
Pancreatic-enteric fistula
- Spontaneous decompression of pseudocyst into adjacent hollow viscera
- Bleeding and sepsis
- Surgery is the treatment
