1. HEPATITIS B (HBV- Hepadenaviridae)
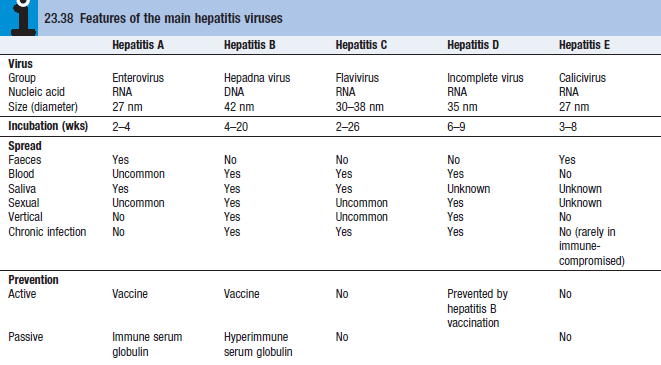
Etiology/epidemiology
- MCC of chronic liver disease and hepatocellular carcinoma (HCC)
- 33% of the population have serological evidence of past or current infection
- Horizontal transmission – IVDU, infected blood products, sex, tattoos
- Vertical transmission – highest risk of ongoing chronic infection
Pathology
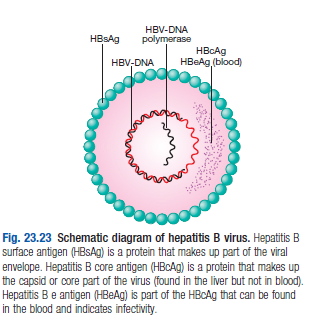
- HBV has a core containing DNA and a DNA polymerase (for viral rep)
- Core of virus is surrounded by surface protein HBsAg
- Chronic hep can lead to cirrhosis or HCC usually after decades
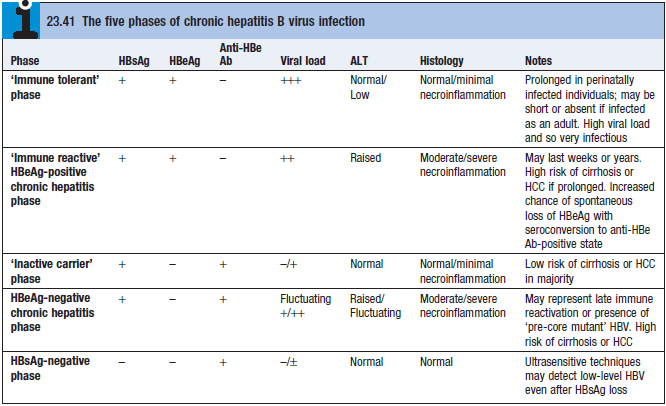
- Chronic HBV infection can be divided into 5 phases (see box)
- The virus is not directly cytotoxic to cells – the immune response to viral Ag displayed on infected hepatocytes that initiates liver injury (CD8 cytotoxic T cells contribute most to liver injury)
Investigations
- Serology
- HBV contains several Ags to which infected pts can make an immune response
- HBsAg – indicator of active infection
- Disappears before jaundice has developed
- Persistence longer than 6 months indicates chronic infection
- Ab to HBsAg (anti-HBs) appears after 3-6 mo and persists for years/permanently
- Anti-HBs implies previous inf (in which case anti-HBc is also present) or previous vaccination (where anti-HBc is not present)
- HBcAg – core antigen
- HBcAg is not found in the blood but Ab to it (anti-HBc) appears early and rapidly reaches a high titre
- anti-HBc is initially of IgM type, with IgG Ab appearing later
- HBeAg – indicator of viral replication
- Its appearance is followed by production of its Ab (anti-HBe)
- Chronic HBV infection is marked by HBsAg + anti-HBc (IgG), usually HBeAg or anti-HBe is also present – indicates continued active rep of the virus in the liver
- Absence of HBeAg – low viral rep
- Exception – HbeAg-negative chronic hepatitis B (AKA pre-core mutant infection)
- In which high levels of viral rep and hepatic necroinflammation occur despite negative HBeAg
Viral load and genotype
- HBV DNA can be measured by PCR in the blood
- Measuring viral load is important to monitor antiviral therapy (usually >105 copies/mL)
- HBsAg- and anti-HBe-positive – <105 copies/mL
- Exception in pts who have a mutation in the pre-core protein – cannot secrete e Ag into serum
- Patients are anti-HBe-positive but have a high viral load and evidence of chr hep
- Mutations common in Far East
- These pts are classified as having HBeAg-negative chronic hep
Management
- No drug can eradicate HBV infection completely
- Goals of treatment – HbeAg seroconversion, reduction in HBV DNA and normalisation of liver functional tests (LFT)
- Indication for treatment – high viral load in the presence of active hepatitis and/or histological evidence of inflam and fibrosis
- Most patients with chronic HBV are symptomatic; develop cirrhosis and HCC after many years
- Monitor patients who do not meet anti-viral treatment criteria
Treatment
- Direct-acting nucleoside/nucleotide antiviral agents
- Inhibit the reverse transcription of pre-genomic RNA to HBV-DNA by HBC-DNA polymerase
- Relapse common if tx withdrawn
- Lamivudine –
- Entecavir + tenofovir – more effective, less viral mutants
- Indicated in HIV pts because of anti-HIV properties
- Interferon-alfa
- Most effective in pts with low viral load
- Contraindicated in pts with cirrhosis, as it may precipitate liver failure
- Side effects are common – fatigue, depression, irritability, BM suppression, autoimmune thyroid disease
- Liver transplant
Prevention
- HBV is x10 more infectious than hepatitis C virus (HCV)
- Engerix (recombinant HB vaccine containing HBsAg)
- Neonates born to HBV infected mothers should be immunised at birth and given immunoglobulin
2. HEPATITIS D (HDV – Deltavirus)
- HDV is an RNA-defective virus, has no independent existence
- Requires HBV for replication, has the same sources and modes of spread
- Can infect pts simultaneously with HBV or can superinfect chronic carriers of HBV
- Simultaneous infections – acute hepatitis, severe but is limited by recovery from HBV
- Chronic infection with HBV + HDV – rapidly progressive chronic hepatitis and eventually cirrhosis
- MC transmission by close personal contact and vertical transmission
Investigations
- HDV contains a single Ag to which infected pts make an Ab (anti-HDV)
- Delta Ag only appears transiently, dx based on detecting anti-HDV
- Simultaneous inf with HBV + HDV followed by full recovery
- Assoc with appearance of low titres of anti-HDV of IgM within a few days of onset
- Superinfection of pts with chronic HBV infection
- Prod of high titres of anti-HDV, initially IgM, and then IgG
Management
- Effective management of HBV prevents HDV
3. HEPATITIS C (RNA flavivirus)
- Acute symptomatic infection is rare, most pts are identified when they develop chronic liver disease
- 80% of pts become chronically infected
- HCV infection identified in individuals who are screened because they have high RFs for infection (IVDU, unscreened blood products, needlestick injury, sharing razors)
Investigations
- Serology and virology
- HCV protein contains several Ags which give rise to Abs in an infected person
- May take 6-12 weeks for Abs to appear
- Hepatitis C RNA can be identified in the blood as early as 2-4weeks
- Molecular analysis
- 6 common viral genotypes
- LFTs – may be normal or show fluctuating serum transaminases between 50-200U/L
- Jaundice is rare, only appears in end-stage cirrhosis
- Liver histology – since serum transaminases are poor predictor of degree of liver fibrosis, biopsy is often needed
Management
- Until recently, DOC was dual therapy with pegylated IFN-a combined with oral ribavirin
- Ribavirin SE – haemolytic anaemia and teratogenicity
- IFN SE – flu-like sx, irritability, depression
- Virological relapse can occur in first 3 mo after stopping tx
- Triple therapy – addition of protease inhibitors (telaprevir/boceprevir)
- Progression from chronic hepaitis to cirrhosis occurs over 20-40 years
- RF – male, immunosuppression (HIV), alcohol misuse
- Once cirrhosis is present, 2-5% per year will develop HCC