- Thrombohemorrhagic disorder – pathologic activation of both the coagulation cascade and fibrinolysis
- Fibrin thrombi occlude the microcirculation throughout the body – produces ischemic damage
- Bleeding occurs from GIT, nose etc – produces anaemia
Pathogenesis
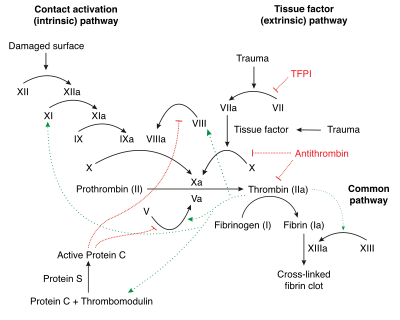
Activation of the coagulation cascade
- Activation of the extrinsic system – occurs by release of tissue thromboplastin from damaged tissues. E.g.
- Massive trauma – RTA, surgery
- Hypovolemic or cardiogenic shock
- Malignancies –
- Obstetric problems – amniotic fluid embolism, placental abruption
- Activation of the intrinsic system – by activation of factor XII by surface contact with collagen secondary to endothelial cell injury. E.g.
- G- septicaemia with release of endotoxins (MCC of DIC)
- Deposition of immune complexes – e.g. SLE
- severe burns or heat stroke
Consequences
- With activation of either extrinsic or intrinsic system, there is ↑thrombin, leading to an ↑conversion of fibrinogen → fibrin
- Fibrin thrombi develop in the microcirculation
- Fibrin thrombi
- Obstruct blood flow – leading to ischemia and infarction
- Consume coagulation factors (I, II, V, VIII) – causing bleeding problems
- Trap platelets – causing thrombocytopenia (contributes to bleeding)
- Development of petechiae and ecchymoses on skin and mucous membranes
- Damage circulating RBCs – producing microangiopathic haemolytic anemia (MHA)
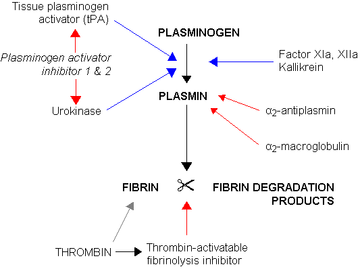
Leads to activation of fibrinolytic system – due to activation of plasminogen by factor XIIa and tPA (+urokinase)
- Causes plasminogen → plasmin
- Function of plasmin
- cleaves insoluble fibrin into FDPs
- degrades factors V, VIII and fibrinogen
Clinical Features
Acute DIC – infections (bacterial sepsis) is MCC
- Haemorrhage CFs – petechiae, ecchymoses, bleeding from nose, GIT, urinary tract
- Widespread thrombosis – digital gangrene
Chronic DIC – malignancies are MCC
- thromboembolism
- Some pts are asymptomatic as there is a balance between clotting and fibrinolytic system
- Liver is able to compensate for the degradation of clotting factors
 Diagnosis
Diagnosis
Coagulation abnormalities
- ↑PT and PTT
- Decreased serum fibrinogen
Platelet abnormalities
- Thrombocytopenia
- Increased bleeding time
Fibrinolysis abnormalities
- Presence of FDPs and D-dimers
Normocytic anemia
- Due to bleeding from skin and GIT
- MHA with schistocytes – due to mechanical damage of RBCs
Treatment
- Correct underlying cause of DIC
- Heparin – to shut off thrombin activity and prevent conversion of fibrinogen to fibrin
- Fresh frozen plasma – to correct multiple coagulation factor deficiencies
- Packed RBCs – to correct anemia
- Platelet transfusion – to correct thrombocytopenia