Pituitary gland is unable to produce significant levels of hormones.
Etiology
- May be isolated or multiple
- (tumour/lesions)
- Pituitary tumours (adenoma) or non-pituitary tumours (craniopharyngioma, meningioma, glioma)
- Causes by genetic, sporadic, autoimmune
- Order of deficiencies (pituitary hormones)
- GH/gonadotropins > Hyperprolactinemia > TSH/ACTH
Clinical features
- 2o hypothyroidism /adrenal failure – tiredness, malaise
- Hypothyroid symptoms
- Hypoadrenalism – hypotension, hyponatremia (brain edema), cadiovascular collapse
- Gonadal deficiency – libido loss, amenorrhea, puberty hair loss, erectile dysfunction
- Hyperprolactinemia – galactorrhoea, hypogonandism
- Chronic panhypopituitarism – pallor with hairlessness
Specific syndromes
- Kallmann – gonadotropin deficiency – KAL1 mut (anosmin)
- Sheehan – postpartum haemorrhagic necrosis
- Pituitary apoplexy – pituitary tumour rapidly enlarging due to infarction
- Empty sella – sella turcica void of pituitary tissue – cisternal herniation
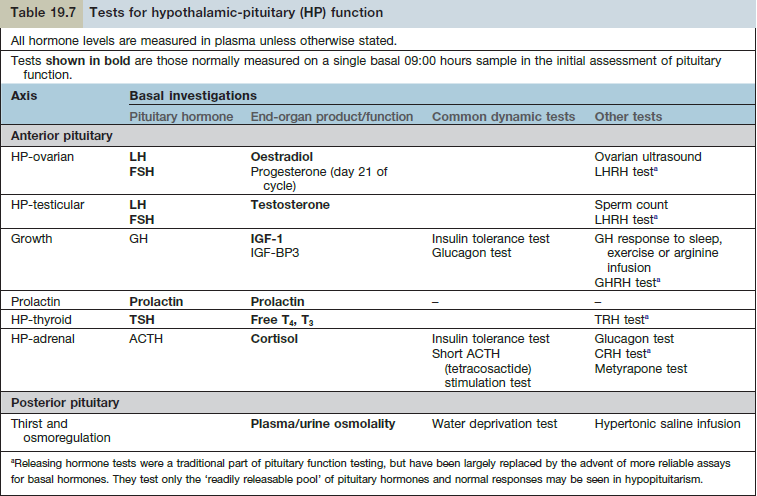
Diagnosis
- Separate tests need to be carried out for each individual hormone axis
- Insulin tolerance test for ACTH and GH
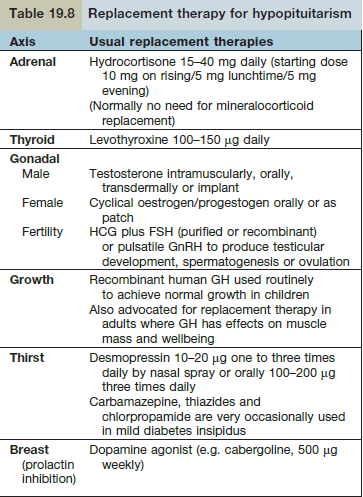
Treatment
- Thyroid and steroids are essential for life
- Glucocorticoid function needs to be adequate before starting thyroid medication – risk of Adrenal crisis
- Glucocorticoid deficiency may Mask diabetes insipidus – becomes apparent after steroid replacement.