- Neoplastic clonal proliferations of lymphocytes
- Can involve LNs, extranodal tissues, or both
- Usually systemic, widely disseminated diseases
- Can be tumours of B or T lymphocytes – B cell tumours MC in US
Epidemiology
- MC in Caucasian men
- MC in 60-70 year olds
- NHLs in children tend to be more aggressive
Etiology
- Genetic predisposition – increased incidence in people with inherited immunodeficiency disorders
- E.g. ataxia-telangiectasia, Wiskott-Aldrich syndrome (XLR disorder characterised by eczema, thrombocytopenia and immune deficiency)
- Pesticides, herbicides
- Viruses – EBV, HTLV-1, HCV
- EBV infects and immortalises B cells and stimulates B cell replication
- Immunosuppression – predisposes to NHL e.g. HIV
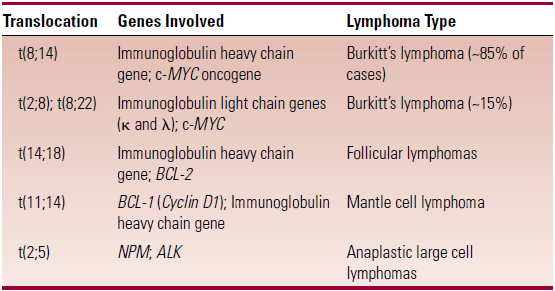
Cytogenetics
- In normal development the genes for lymphocyte antigen receptors (Igs for B-cells, TCR for T-cells) go through a process of genetic recombination
- In this process reciprocal translocations can occur, predisposing to NHL and other malignancies
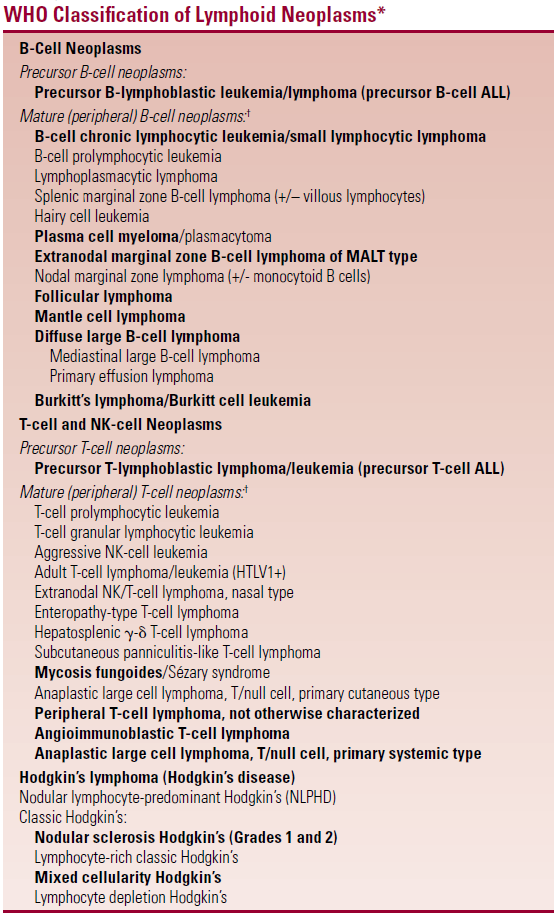
Classification – see WHO classification at end
- Two most common are
- Diffuse large B-cell lymphomas
- Follicular lymphomas, t(14:18)
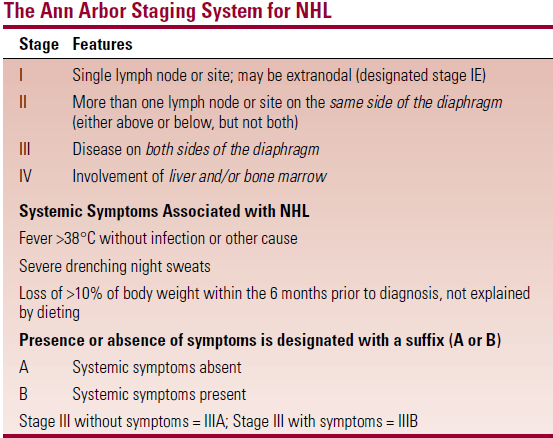
Staging
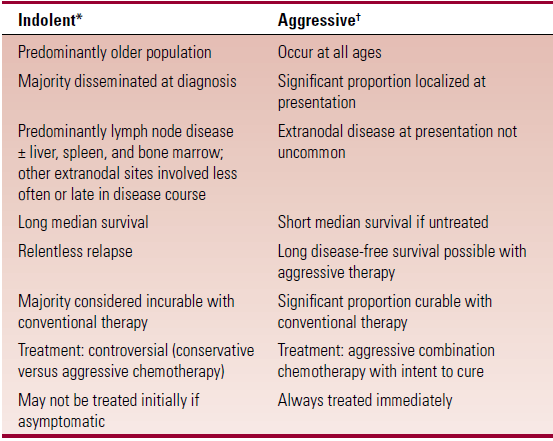
Indolent vs Aggressive NHLs
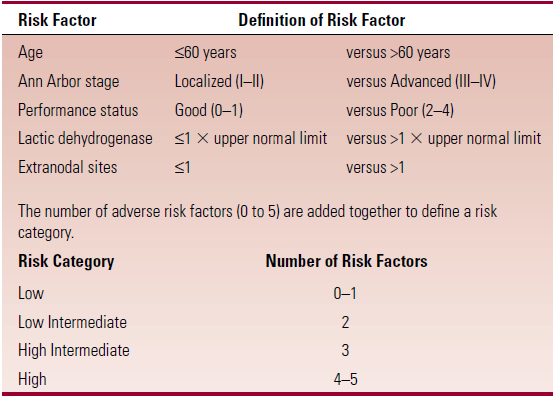
Prognostic factors – summarised in the International NHL Prognostic Index
Diagnosis
- Histology
- Immunophenotyping – by flowcytometry
- Detection of Ig light chain restriction (imbalance in expression of κ and λ light chains on lymphocytes, rather than the normal 2:1 ratio of κ to λ) suggests a clonal B-cell population – i.e. a B-cell malignancy
- Cytogenetics
- Antigen receptor gene rearrangement studies
- Excision biopsy w/ immunohistchem
Specific lymphoma types
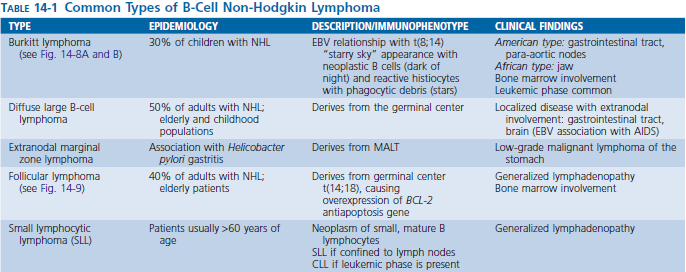
Diffuse large B-cell lymphomas – MC type of lymphoma
- Most aggressive if untreated
- Variable histologic appearance
- If CD-20 +ve use rituximab
Follicular lymphomas
- Subdivided into 4 histologic grades
- Follicular, predominantly small cleaved cell (grade I)
- Follicular, mixed small cleaved and large cell (grade II)
- Follicular, predominantly large cell (grade III)
- Grade I + II are indolent with long survival
- Translocation [t(14;15)] – over expression of BCL-2, inhibits apoptosis
Small lymphocytic lymphoma
- Tissue based equivalent of CLL – only distinction is based on absence of lymphocytosis in SLL (<5000 ly/μL)
- Low grade
- Expresses CD5 (T-cell marker) – only other B-cell lymphoma to express CD5 is mantle cell lymphoma
Lymphoma of Mucosa-Associated lymphoid tissue (MALT)
- MALT lymphomas are MC type of extranodal lymphoma – MC in stomach
- Also in salivary glands, breasts, thyroid
- Localised at diagnosis – systemic dissemination occurs late
- Indolent
- Relapses after therapy frequently occur at other MALT sites
- Chronic gastritis caused by H.pylori is implicated in gastric MALT
Mantle cell lymphoma
- MC in older males
- Most cases are advanced at diagnosis, with BM involvement
- Characterised by small cells with nuclear irregularity
- Translocation [t(11;14)] is implicated
- Expresses CD5
Burkitt’s lymphoma
- Very high grade NHL
- MC in Africa
- MC in children
- Burkitt cell leukemia – is the leukemic equivalent. Their behaviour and treatment are the same
- Strong association with EBV and malaria in Africa
- Universal association between BL and the translocation of the c-MYC proto-oncogene to one of the Ig gene (heavy or light chain)
- t(8;14) – most common translocation
- c-MYC on C8 is translocated to the Ig heavy chain gene on C14
- over expression of c-MYC gene results in very high proliferation rate of cells
- t(8;14) – most common translocation
- African presentation – big, rapidly growing jaw mass in young child
- US presentation – most pts present with intra-abdominal disease
T-cell lymphomas
- Most are peripheral T-cell lymphomas
- Compared to B-cell lymphomas, those of T-cell have a higher incidence of extranodal disease and are at an advanced stage at diagnosis
- Most are associated with B symptoms (systemic sx)
- Worse prognosis
Treatment
Indolent lymphomas
- Watch and wait if pt is asymptomatic
- Chemotherapy
- COPP – cyclophosphamide, oncovin (vincristine), prednisone, procarbazine
- Radiation
- Interferon
- Fludarabine – for relapses
- Rituximab – anti CD20
Aggressive lymphomas
- Chemotherapy
- CHOP – cyclophosphamide, hydroxydaunorubicin (doxorubicin), oncovin, prednisone
- Radiation
- Stem cell transplant