- Jaundice – yellow staining of the skin, sclera and mucous membranes by bilirubin
- Normal level of bilirubin is <1.0 mg/dl
- Jaundice manifests when levels are 2.5-3.0 mg/dl
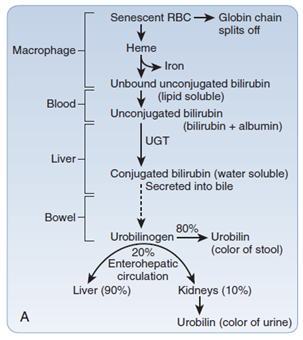
Metabolism of bilirubin
- Bilirubin is a bile pigment produced by the breakdown of red blood cells
- Bilirubin is conjugated within the liver by the enzyme UDP-glucuronyl transferase
- Conjugated bilirubin is water soluble
- It is then secreted into bile
- Bilirubin enters the intestinal tract via bile
- The intestinal bacteria converts it into urobilinogen
- 80% of urobilinogen is then converted to stercobilinogen
- 20% of urobilinogen is reabsorbed by enterocytes
- Most of it is transported back to the liver – enterohepatic circulation
- Some of it is filtered into the kidney
Causes of jaundice
Pre-hepatic
- Jaundice is due to excessive hemolysis which overwhelms the liver’s ability to conjugate bilirubin
- Leads to unconjugated hyperbilirubinemia
- Examples
- Haemolytic anemia
- Gilbert’s syndrome – decreased glucuronyl transferase
- Criggler-Najjar syndrome – absent glucuronyl transferase
Hepatocellular
- Jaundice is due to dysfunction of the hepatocytes – the liver loses its ability to conjugate bilirubin
- In a cirrhotic liver, there is also compression of the intra-hepatic biliary tree – leading to obstruction
- For this reason, there is increase in both unconjugated and conjugated bilirubin in the blood
- Examples
- Alcoholic liver disease
- Viral and autoimmune hepatitis
- Primary sclerosing cholangitis
- Hepatocellular carcinoma
Post-hepatic (obstructive)
- Obstruction of biliary drainage
- Because the liver has already conjugated the bilirubin there will be conjugated hyperbilirubinemia
- Examples
- Intraluminal – gallstones
- Intramural – cholangiocarcinoma, strictures
- Extramural – pancreatic cancer, lymphomas
- Causes ↑ALP and GGT
Clinical features
- Yellowish discolouration of the sclera and skin
- Dark urine
- Pale, fatty stools
- Itchiness
Investigations
Blood markers
- AST:ALT ratio – over 2 indicates alcoholic liver disease; ratio of 1 indicates viral hepatitis
- ALP – raised in biliary obstruction
- Isolated rise in ALP without GGT elevation – indicates malignancies
- GGT – more specific for biliary obstruction than ALP
Liver screen
- Hepatitis – A, B, C, E
- CMV, EBV
Imaging
- Ultrasound abdomen
- MRCP – to visualise biliary tree
- Liver biopsy
Treatment
- Depends on the underlying cause
Obstructive jaundice
- ERCP – to remove gallstone
- Stenting of the common bile duct
- Symptomatic treatment for itching – cholestyramine, antihistamine
- Manage coagulopathy – vitamin K, fresh frozen plasma
