Epidemiology
- More common in men
- Peak incidence is >65 years old
- African-American people are affected more
- Poor prognosis at time of presentation – usually local and distant metastasis
- Mean survival time for adenocarcinoma is 9-12 months
Etiology
- Cigarette smoking
- Processed meats – containing N-nitroso compounds
- Diabetes mellitus, chronic pancreatitis
- Alcohol, caffeine
- Peutz-Jeghers syndrome
Pathophysiology
- Carcinoma arises from the exocrine portion of the pancreas
- Most commonly from pancreatic acinar cells and ductal epithelium
- Alcohol etiology is most common in carcinoma of head of pancreas
Metastasis
- From the body and tail of pancreas it metastasises to parapancreatic and splenic lymph nodes
- From the head of pancreas it metastasises to the hepatoduodenal ligament
- Local spread – to adjacent structures i.e. duodenum, portal vein, superior mesenteric vein
- Distant spread – liver, lungs, adrenals, brain, bone
Clinical features
- Initially, vague symptoms – anorexia, weight loss, abdominal discomfort, pain after eating
- First significant symptom – mechanical jaundice
- Occurs when tumour infiltrates the cystic duct
- Pain in upper abdomen and back
- Troisier’s sign – palpable Virchhow’s node
- Due to thoracic duct obstruction
- Also seen in cancer of the lungs, oesophagus, stomach
- Courvoisier sign – a palpable, non-tender gallbladder in the presence of mild jaundice suggests malignancy
- Trousseau’s sign – migratory superficial thrombophlebitis
- Sister Mary Joseph nodule – palpable nodule bulging into umbilicus as a result of metastases in pelvis/abdomen
- Intestinal obstruction – tumour in head of pancreas compresses duodenum
Investigations
- CT with contrast
- MRI – for metastases
- Cholangiography – to look for infiltration of major pancreatic duct
- CEA tumour marker – useful for follow-up (if CEA levels don’t decrease after resection, it signifies an unsuccessful resection)
Treatment
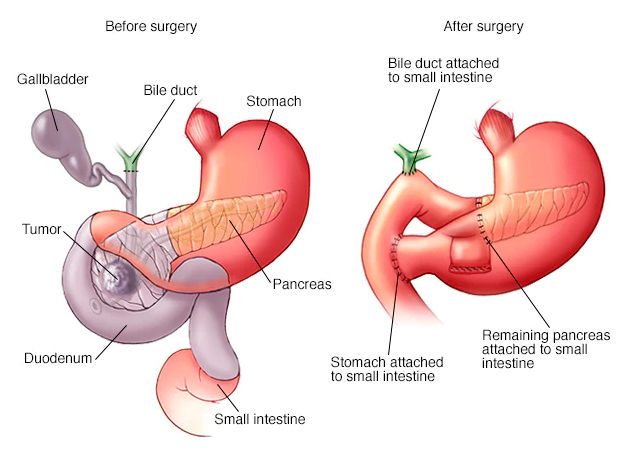
- Whipple’s operation (see pic) – pancreaticoduodenectomy
- 3 anastomoses – pancreaticojejunostomy, choledojejunostomy, gastrojejunostomy