- Definition – ulcer in lower stomach or duodenum. Can be acute or chronic; both penetrate the muscularis mucosae but acute ulcer shows no sign of fibrosis. Anterior penetrates and posterior bleeds.
Etiology
- Gastric ulcer (GU)
- Imbalance between protective and damaging factors of gastric mucosa
- Atrophic gastritis, bile reflux, gastric stasis, abnormalities in acid and pepsin secretion
- Smoking, alcohol, NSAIDs, steroids
- H. Pylori – G-, spiral, multiple flagella
- Low socioeconomic group
- Duodenal ulcer (DU)
- MC in blood group O +ve
- Stress, anxiety
- H.pylori infection
- NSAIDs, steroids
- Endocrine causes – Zollinger-Ellison syn, MEN syn, hyperparathyroidism
Pathogenesis – commonly H pylori/NSAIDs
H.pylori
- Strongly associated with H.pylori infection – increases with age and developing countries
- Person to person contact
- Most colonised people are healthy and asymptomatic
- 90% of DU and 70% of GU pts are infected
- The remaining are caused by NSAIDs, especially in developed countries
- Motile – allows it to burrow and live beneath mucus layer adherent to the epithelial surface
- Adhesion molecule BabA binds to Lewis b Ag on epithelial cells
- Releases urease to neutralise any acidity >> produces ammonia >> raises the pH around bacterium
- Causes chronic gastritis by provoking a local inflam response – depends on expression of
- cagA gene – injected into epithelial cells, interacts with cell-signalling pathways involved in cell replication and apoptosis
- vacA gene – pore forming protein, causes increased cell permeability, efflux of micronutrients from the epithelium, induction of apoptosis and suppression of local immune cell activity
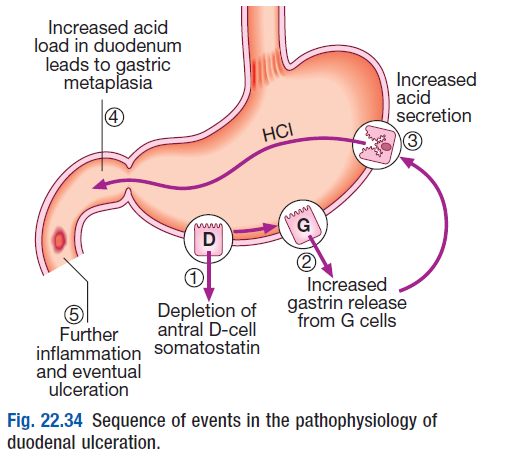
- causes increases gastrin release from G cells >> hypergastrinemia >> increased acid prod by parietal cells
- rarely can cause pangastritis >> gastric atrophy and hypochlorhydria
- allows other bacteria to proliferate within the stomach >> predisposes to gastric cancer
- effects of H.pylori are more complex in GU than DU
 NSAIDs
NSAIDs

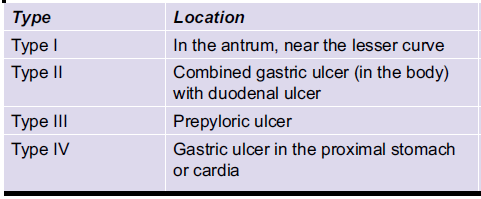
Gastric Ulcer
Duodenal Ulcer
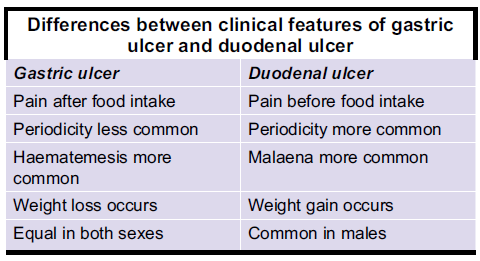
Clinical features
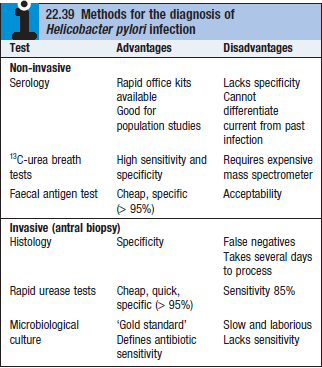
Diagnosis
- Barium meal XR – niche + notch (GU), absence of duodenal cap (DU)
 Gastroscopy (need to stop PPI 2 weeks before procedure)
Gastroscopy (need to stop PPI 2 weeks before procedure)- Forrest classification is used to assess risk and intervention by endoscopic procedures.
- Abdominal US
- Biopsy – on all gastric ulcers
- Ulcers on greater curvature assumed to be malignant unless proved otherwise
- FBC – T2/T3 ulcers show HCl hypersecretion
Differential diagnosis
- Hiatus hernia, cholecystitis, chronic pancreatitis, dyspepsia, carcinoma stomach, gastrinoma, cushing/curling ulcers, Crohns, TB, Zollinger-Ellison syndrome
Treatment
- H.pylori eradication
- PPI + 2 abx of: amoxicillin, clarithromycin and metronidazole for 7d
- Omeprazole 20mg + amoxicillin 1g, clarithromycin 500mg
- Quadruple therapy – in case of eradication failure
- PPI, bismuth subcitrate, metronidazole, tetracycline for 14d (OBMT)
- PPI + 2 abx of: amoxicillin, clarithromycin and metronidazole for 7d
- General measures – cig, aspirin, NSAIDs should be avoided
- Antacids – aluminium hydroxide
- Surgery –
- Partial gastrectomy with Billroth I anastomosis (gastroduodenostomy)
- Highly selective vagotomy may be performed to decrease acid secretion. (parietal cells ligated)
Complications
- Haemorrhage (usually DU and posterior, use ROCKALL score to assess rebleeding risk) – leads to shock
- Perforation (usually GU and anterior) – leads to chemical peritonitis
- Gastric outlet obstruction (chronic DU)
