- Chronic abnormal communication running outwards from anorectal lumen to an external opening on
- The skin of perineum
- The skin of buttock
- The skin of vagina
- The fistula usually originates in the infected crypt (internal opening) and tracks to the external opening, usually at the site of prior drainage
- The course of the fistula can often be predicted by the anatomy of the previous abscess
Clinical features
- Intermittent purulent discharge – pain until discharge is completed
- Skin irritation
- Anorectal sepsis
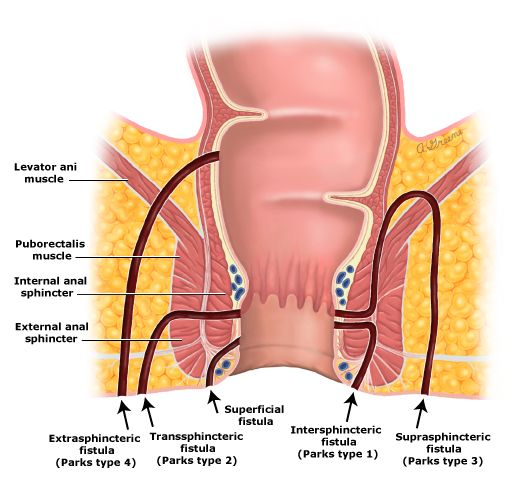
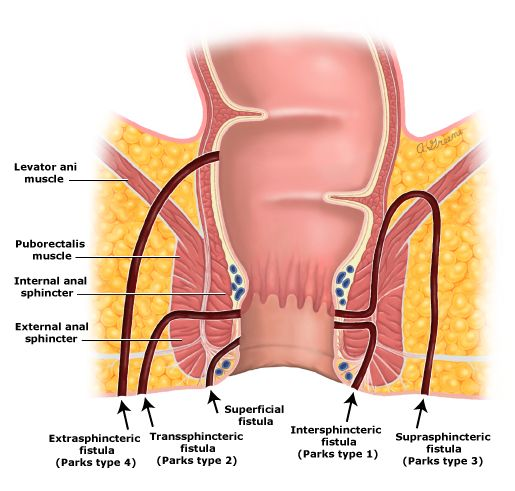
Classification – Parks Classification
- 1 – Intersphincteric (70%)
- Found between internal and external sphincter
- 2 – Transphincteric (23%)
- As a result of ischio-rectal abscess
- Extends through both internal and external anal sphincter
- 3 – Suprasphincteric (2%)
- Originates from the intersphincteric space and tracks up and around the entire external sphincter
- 4 – Extrasphincteric (5%)
- Originates in rectal wall, tracks around both sphincters
- Exits laterally in the ischiorectal fossa
- The rule is used to predict the trajectory of a fistula tract depending on the location of the external opening in relation to the transverse anal line
- If the external opening is located anterior to the transverse anal line – the fistula will have a straight tract
- If the external opening is located posterior to the transverse anal line – the fistula will have a curved tract
- May present with multiple external openings all connected to a single internal opening
Investigations
- Fistulography + CT
- MRI – gold standard
- Proctosigmoidoscopy under general anaesthesia
- Dilute hydrogen peroxide instilled via the external opening – demonstrates the site of internal opening
Treatment
- Treat the concomitant abscess
- Sitz bath and fibre therapy
Fistulotomy – for low anal fistulas
- Probe is inserted into tract (from external to internal)
- Base of wound and granulation tissue removed
- Surgery for complex fistula – i.e. high transphincteric, suprasphincteric, extrasphincteric
- Striated muscle superficial to the fistula tract is encircled with seton and tied
- It is left in situ to create ischaemic necrosis
- Divides the muscle slowly without allowing it to spring apart, avoiding gutter deformity
- Allows fistula to granulate and heal from above and close completely
Other procedures
- Fibrin glue – easy to use, avoids sphincter division
- Tract is debrided, then glue is injected
- Anal fistula plug – better than glue
85
Perianal Fistula
- Chronic abnormal communication running outwards from anorectal lumen to an external opening on
- The skin of perineum
- The skin of buttock
- The skin of vagina
- The fistula usually originates in the infected crypt (internal opening) and tracks to the external opening, usually at the site of prior drainage
- The course of the fistula can often be predicted by the anatomy of the previous abscess
Clinical features
- Intermittent purulent discharge – pain until discharge is completed
- Skin irritation
- Anorectal sepsis
Classification – Parks Classification
- 1 – Intersphincteric (70%)
- Found between internal and external sphincter
- 2 – Transphincteric (23%)
- As a result of ischio-rectal abscess
- Extends through both internal and external anal sphincter
- 3 – Suprasphincteric (2%)
- Originates from the intersphincteric space and tracks up and around the entire external sphincter
- 4 – Extrasphincteric (5%)
- Originates in rectal wall, tracks around both sphincters
- Exits laterally in the ischiorectal fossa
Goodsall’s rule
- The rule is used to predict the trajectory of a fistula tract depending on the location of the external opening in relation to the transverse anal line
- If the external opening is located anterior to the transverse anal line – the fistula will have a straight tract
- If the external opening is located posterior to the transverse anal line – the fistula will have a curved tract
- May present with multiple external openings all connected to a single internal opening
Investigations
- Fistulography + CT
- MRI – gold standard
- Proctosigmoidoscopy under general anaesthesia
- Dilute hydrogen peroxide instilled via the external opening – demonstrates the site of internal opening
Treatment
- Treat the concomitant abscess
- Sitz bath and fibre therapy
Fistulotomy – for low anal fistulas
- Probe is inserted into tract (from external to internal)
- Base of wound and granulation tissue removed
- Surgery for complex fistula – i.e. high transphincteric, suprasphincteric, extrasphincteric
Seton technique – for high fistulas
- Striated muscle superficial to the fistula tract is encircled with seton and tied
- It is left in situ to create ischaemic necrosis
- Divides the muscle slowly without allowing it to spring apart, avoiding gutter deformity
- Allows fistula to granulate and heal from above and close completely
Other procedures
- Fibrin glue – easy to use, avoids sphincter division
- Tract is debrided, then glue is injected
- Anal fistula plug – better than glue
