Pleural Diseases
1. PNEUMOTHORAX (PT)
- Presence of air in the pleural space
- Etiology
Pathogenesis
- Closed pneumothorax – communication between the airway and the pleural space seals off as the lung deflates and doesn’t re-open
- Pleural pressure remains negative
- Spontaneous reabsorption of air an re-expansion of lung occurs in days-weeks
- Open pneumothorax – communication fails to seal, air continues to pass freely between bronchial tree and pleura
- E.g. a bronchopleural fistula
- Can facilitate transmission of infection from airways into the pleura and lead to empyema
- MC after rupture of an tuberculous cavity or lung abscess into the pleura
- E.g. a bronchopleural fistula
- Tension pneumothorax – communication between the airway and pleura acts as a one way valve
- Allows air to enter the pleura during inspiration but not to escape during expiration
- Large amount of trapped air accumulates – intrapleural pressure rises above atmospheric pressure
- Can cause mediastinal displacement to the opposite side, with compression of the opposite normal lung
Clinical features
- Sudden onset unilateral pleuritic chest pain
- Breathlessness
- Combination of absent breath sounds + resonant percussion is diagnostic of PT
- Tension PT – rapidly progressive breathlessness, tachycardia, hypotension, cyanosis, mediastinal shift
Diagnosis
- CXR – sharply defined edge of deflated lung; absent lung markings external to edge; mediastinal shift
- CT – not routine; indications are underlying lung disease or uncertain diagnosis
Treatment
- Primary PT in which the lung edge is <2cm away from chest wall – resolves without intervention
- Percutaneous needle aspiration of air
- Intercostal tube drainage – for patients with significant underlying lung disease
Tension PT
- Needle decompression – temporary measure before chest drain can be placed
- In 2nd intercostal space, mid clavicular line
- Chest drain – with distal end connected to an underwater seal
- 4th/5th intercostal space in the mid axillary line
2. EMPYEMA
- Collection of pus in pleural cavity – large amount of neutrophils are present
Etiology
- Empyema is most commonly due to bacterial pneumonia or TB
- Other causes
- Infection of haemothorax following trauma/surgery
- Oesophageal rupture
- Rupture of subphrenic abscess
Pathogenesis
- Pleural spaces are covered with a thick inflammatory exudates
- Due to ↑pressure, the pus can rupture into a bronchus – causing bronchopleural fistula
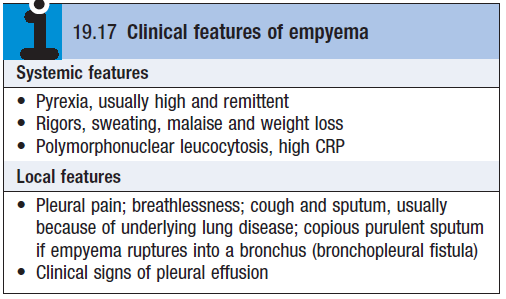
Clinical features
Diagnosis
- CXR – can be indistinguishable from pleural effusion
- CT
- USS
Treatment
- Chest tube drainage
- Antibiotics
3. MESOTHELIOMA
- Malignant pleural tumour
- Etiology – past asbestos exposure
- Clinical features – increasing breathlessness due to pleural effusion; chest pain
- As tumour progresses it can invade the lung parenchyma, mediastinum and pericardium
- Poor prognosis – therapy is mostly palliative
- Chemotherapy
- Radiotherapy
- Pleurodesis – to manage pleural effusions, obliteration of pleural cavity.
