- Frequently complicates cirrhosis
 Normal hepatic venous pressure gradient – 5-6mmHg
Normal hepatic venous pressure gradient – 5-6mmHg- PHTN is >10mmHg – causes increased risk of variceal bleeding
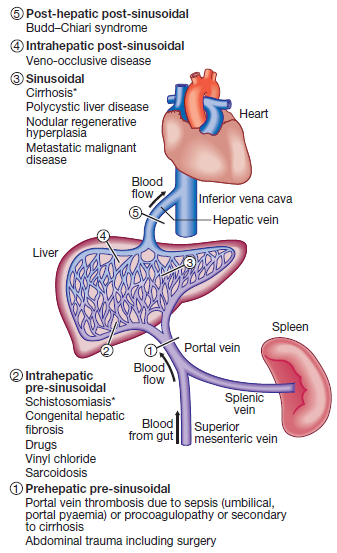
Etiology – see diagram
-
- Childhood PHTN – extrahepatic portal vein obstruction MCC
- Adult PHTN – cirrhosis MCC
Pathophysiology
- Increased portal vascular resistance leads to ↓portal blood flow to liver
- Leads to development of collateral vessels
- allows blood to bypass the liver and enter systemic circ directly
- Portosystemic shunting occurs – esp in GIT (oesophagus, stomach, rectum); anterior abdominal wall; renal, lumbar, ovarian & testicular vasculature
- As collaterals form, >50% of portal blood flow may be shunted directly to systemic circulation
Clinical features
- Result from portal venous congestion and collateral vessel formation
- Splenomegaly – cardinal finding
- Collateral vessels on anterior abdominal wall
- caput medusae – engorgement of paraumbilical veins
- Collateral formation occurs in oesophagus, stomach, rectum – varices
- Source of severe bleeding
- Can be aggravated by use of NSAIDs
- Fetor hepaticus – thiols pass directly to the lungs as a result of portosystemic shunting
- Results in musty breath
Investigations (dx can be made clinically)
- Portal venous pressure measurement – to differentiate between pre-sinusoidal and sinusoidal forms
- Balloon catheter inserted via the IVC into the hepatic vein and then the hepatic venule to measue WHVP (wedged hepatic venous pressure)
- Thrombocytopenia – due to hypersplenism
- Endoscopy – to detect oesophageal varices
- CT/MRI angiography – identify extent of portal vein clot
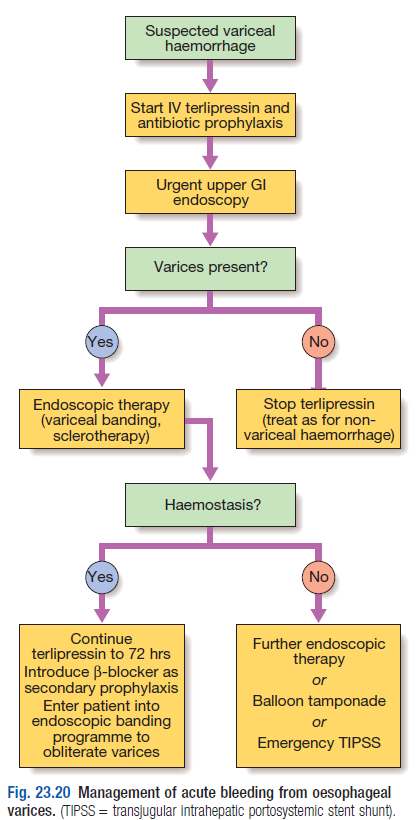
Management (prevention/control of variceal bleeding)
- Primary prevention – non bleeding varices identified at endoscopy, reduce PVP by – propranolol (80-160mg/d)
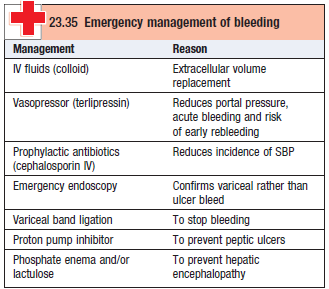
- Managing acute variceal bleeding (see table)
- Aim – restore circ with blood and plasma, because shock reduces liver BF and deteriorates liver function
- Terlipressin [2mg IV qid] – vasopressin analogue, splanchnic vasoconstrictor
- reduces portal BF and hence reduces portal pressure
- If hemodynamically stable w/ FFP, Vit K, platelets
- Band ligation/sclerotherapy – most widely used treatment
- Balloon tamponade – Sengstaken-Blakemore tube with 2 balloons that exert pressure in the fundus of the stomach and in the lower oesophagus (to control life threatening variceal bleeding)
- TIPSS – transjugular intrahepatic portosystemic stent shunting
- Stent placed between portal and hepatic vein via internal jugular v
- Oesophageal resection – last resort, high mortality