 Epidemiology
Epidemiology
- ⅓ of world pop infected with TB
- MC in Africa and Asia
- Co-infection with HIV – gives rise to MDR-TB
Risk factors
- Immune deficiency – HIV, corticosteroid therapy, DM, malnutrition
- Lifestyle – IVDU, homelessness
Etiology
- M.tuberculosis (MTB), bovis, africanum, microti
- Obligate aerobes and facultative intracellular pathogens
- Slow growing acid-fast bacilli
Pathogenesis
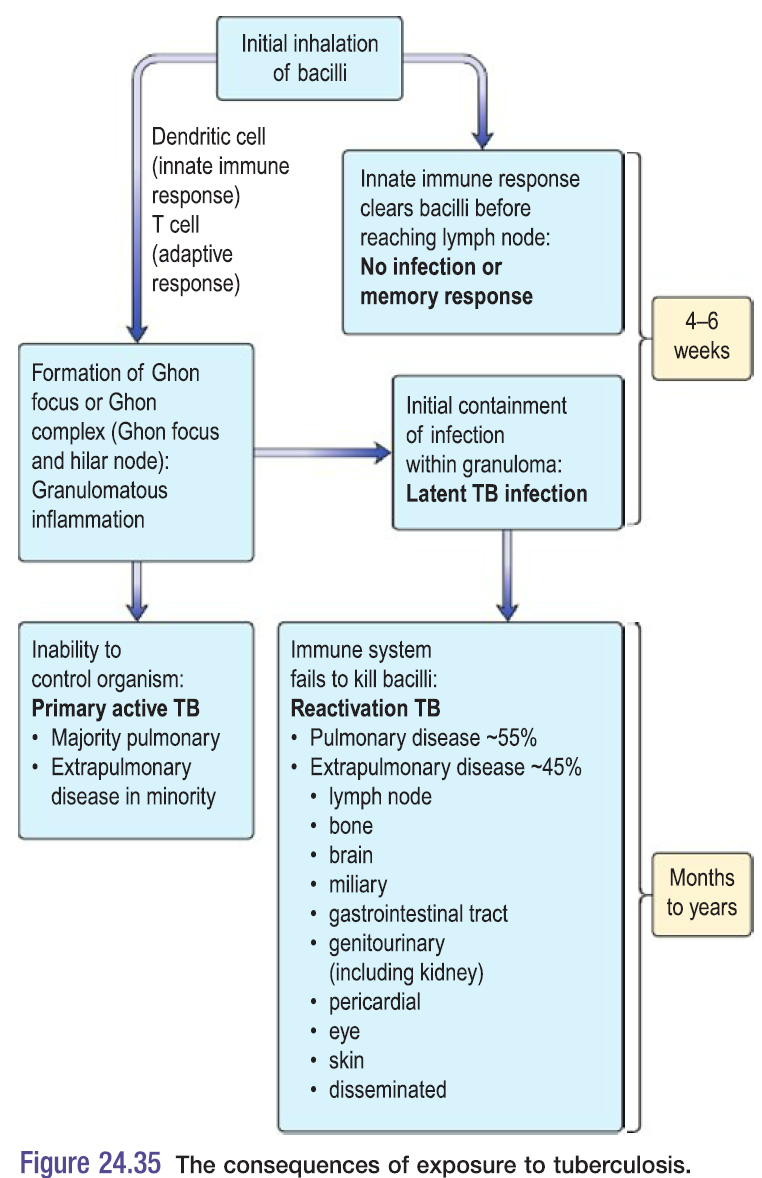
Primary TB
- First infection with MTB
- MTB inhaled into lungs → ingested by alveolar M → bacilli proliferates inside the M → release of chemoattractants + cytokines → inflammatory cell infiltrate reaches the lung → drains hilar LNs
- M present the Ag to T cells → cellular immune response
- Delayed HSR type 4 – results in tissue necrosis + granuloma
- Granulomatous lesion
- Has central caseating necrosis
- Surrounded by epitheloid cells + Langerhans giant cells
- Caseated areas eventually heal – become calcified
- These calcified nodules contain bacteria which can lie dormant for years – called a Ghon focus
- Combination of primary lesion + region lymph node – called a Primary complex of Ranke
- CXR of Ghon focus – small, calcified nodule in mid-zone of the lung
Latent TB
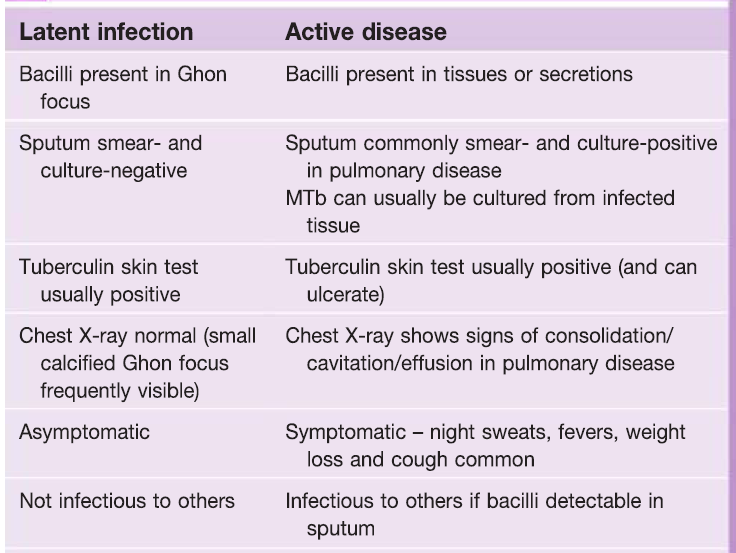 In most people infected by MTB the immune system contains the infection – pt develops cell-mediated immune memory to the bacteria
In most people infected by MTB the immune system contains the infection – pt develops cell-mediated immune memory to the bacteria- Comparison of latent and active TB – see box
Reactivation TB (secondary)
- Most TB cases are due to reactivation of latent infection
- Factors implicated in reactivation – HIV co-infection; Immunosuppressant treatment – chemo, corticosteroids; DM; end stage chronic kidney disease
Clinical features
Pulmonary TB
- Productive cough ± haemoptysis
- Pleuritic pain, pleural effusion
- Systemic symptoms – WL, fever, night sweats
Lymph node TB
- 2nd most common site for TB infection – extrathoraxic nodes are most often involved
- Firm, non-tender enlargement of cervical or supraclavicular node
- Overlying skin is indurated
- Sinus tract formation with purulent discharge – collar stud abscess
Miliary TB
- Due to haematogenous spread
- Systemic symptoms, hepatosplenomegaly, headache (tuberculous meningitis)
- Anemia + leucopenia indicate bone marrow involvement
- CXR shows small (1-2mm) lesions throughout lungs
Other types of TB
- Gastrointestinal TB
- Systemic symptoms; palpable RIF mass
- CT – mesenteric thickening, abdominal lymphadenopathy
- Ascites – exudative fluid
- Pericardial disease
- Pericardial effusion
- Constrictive pericarditis
- SOB, ↑JVP, hepatomegaly, peripheral edema
- CNS disease
- TB meningitis – rapidly fatal
- Bone + joint disease
- Spine is MC site – Pott’s disease
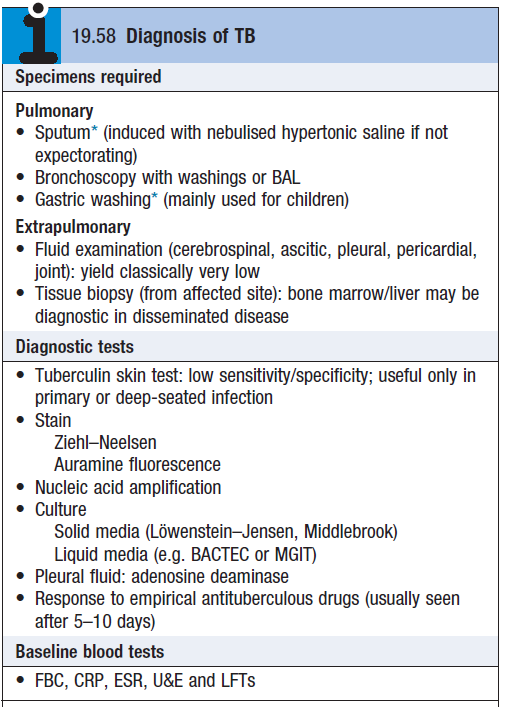
Diagnosis
- See box
- Mantoux test – used to screen high risk people
- Intradermal injection of 10 Tuberculin units
- Positive test – 5-15mm induration after 48-72hrs
- False positives can occur in people who have had the BCG vaccine
- Interferon Gamma Release Assay (IGRA) – unaffected by prior vaccination
- Lumbar puncture – >2g/L protein, <50% glucose
- Nucleic acid amplification – distinguish MTB from Non MTB
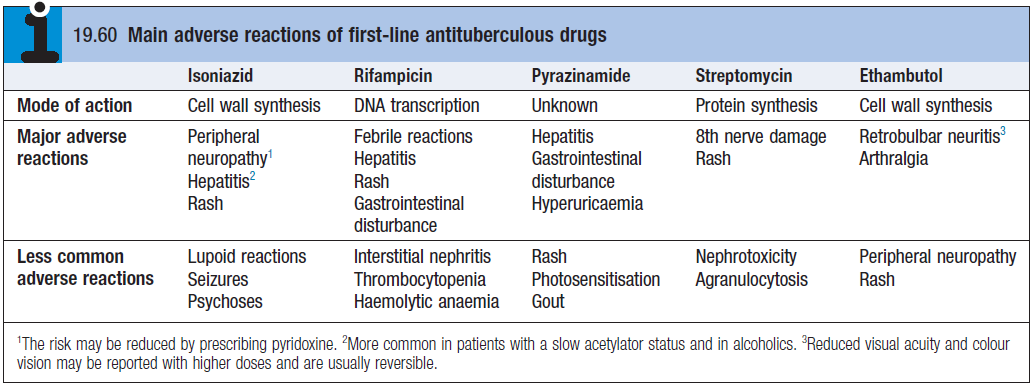
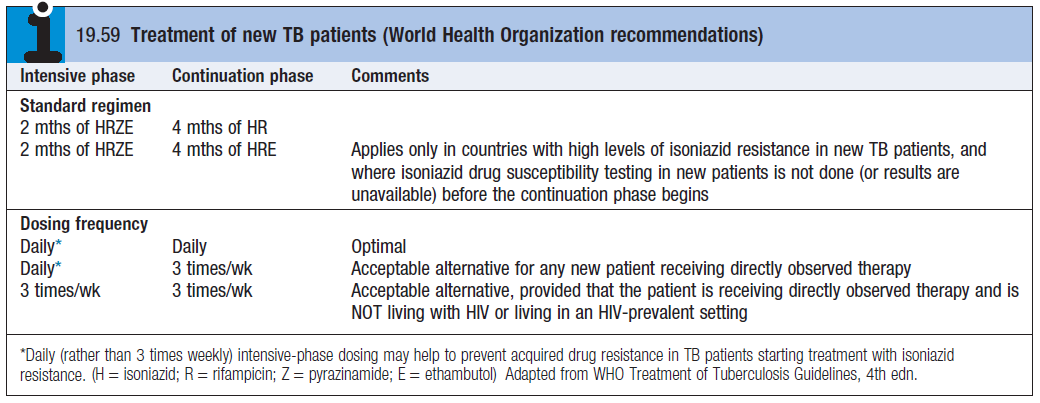
Treatment
- DOT – supervised admin 3 times a week
- BCG vaccine – live attenuated. Intradermal injection
- Pyridoxine [10mcg/day] for pregnant women and B6 deficiency (isoniazid)
- 12 month regimen for meningeal TB – include corticosteroids for inflammation
- Rifampicin – liver inducer (increase in bilirubin and decrease oral contraceptive pill)