Autoimmune disorder, antibodies against IgG Fc region (rheumatoid factor – RF) and citrullinated peptide (ACPA). This leads to persistent synovitis causing chronic symmetrical polyarthritis and systemic inflam.
Epidemiology / etiology
- Females (before menopause) 3x more likely and onset age is 30-50y
- Gender preponderance is equal after menopause. Sex hormones may be indicated.
- HLA-DR4 and smoking is implicated.
Immunology and pathology
Invasion of RA into local tissues and joints causes an overexpression of TNF leading to synovitis and joint destruction. Recruitment and interaction of Mθ, T and B cells (due to chemo attractants secreted by joints) drives TNF and IL-6 upregulation.
Imbalance of specific cells causes immune dysfunction
- B cells – activated by Mθ and T cells in the synovium. Essentially B cells produce IgM and IgA antibodies against RF antigen (IgG Fc). RF has the capacity to self-aggregate and form immune complexes as they contain IgG – Fc. Leading to further cytokine expression (IL-1/8)
- Synovial cells – in RA synoviocytes are abnormal producing a large amount of pro-inflam cytokines.
- T cells, osteoclasts and synovial fibroblasts may also play a role in pathology.
Normally the Synovium is thin and composed of synovio-fibroblasts and Mθ, however in RA the aberrant activation of these cells leads to thickening of the membrane. Inflammatory infiltration causes increased vascularity, permeability and thickening permitting the progression of joint effusion. Hyperplastic Synovium extends over the joint margins ( pannus ) and the synovitis causes to damage of the underlying cartilage. This results in ineffective nutrient exchanging making the cartilage thin. Subsequently the bone is exposed and susceptible to erosion.
RF and ACPA
- IgM-RF not diagnositic of RA but good prognosis predictor.
- Anti-CCP antibodies better predictor of disease transition from transient inflam arthritis to persistent synovitis/RA
Clinical features
- Rheumatoid arthritis – slow progressive symmetrical, peripheral polyarthritis
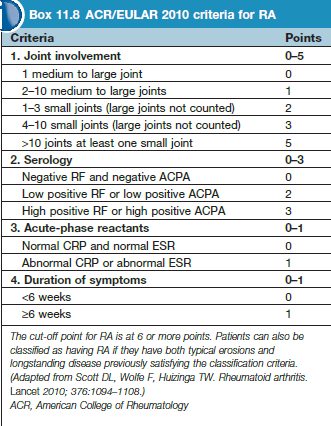
- Criteria to select pts for early tx – 1 joint swollen for >6w, no history of trauma or spondyloarthritis
- Poor prognosis – female, symmetrical joints, >30 min morning stiffness, >4 joints, CRP>20, RF/ACPA +ve
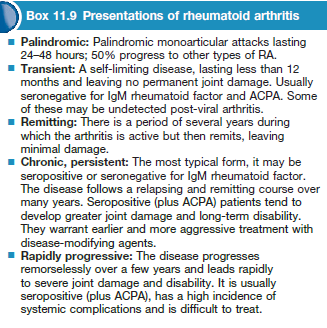
- Other presentations – seronegative RA (affects wrists, better prog), Palindromic rheumatism (short episodes of monoarthritis but resolve completely – may progress to chronic rheumatoid synovitis
Complications
- Septic arthritis, amyloidosis (secondary AA), ruptured tendon, ruptured joints baker cysts , spinal cord compression.
Joint involvement
- Hands and wrists – ulnar deviation, boutonniere deformity, swan-neck deformity
- Shoulders, elbow, feet (early manifestation) – hammer toe deformity, valgus ankle
- Knee – massive synovitis and effusions, increase risk of popliteal cyst, cartilage and joint erosion.
- Hips and cervical spine sometime affected
Non joint involvement
- Lungs – bronchiectasis, bronchiolitis, pleural effusion, fibrosing alveolitis, Caplan syndrome
- Vasculitis – nail fold infarcts, necrotising arteritis, mononeuritis
- Heart/CNS – pericarditis, endocarditis, compression neuropathies,
- Eyes – sjogen syndrome, scleritis, scleromalacia
- Kidney – amyloidosis, nephrotic syndrome, chronic kidney disease
- Felty syndrome – splenomegaly, neutropenia, RA (HLA-DR4)
- Anaemia – noromocytic /normochromic
Diagnosis
- FBC, ESR, Serology, XR, aspiration, Doppler US (persistent synovitis, therapy)
Treatment
- NSAID – paracetamol is best. Must be used.
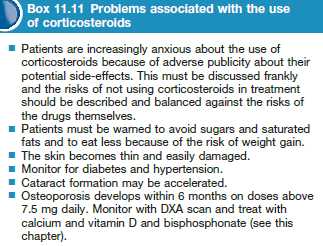
- CS – intra-articular, intramuscular, oral
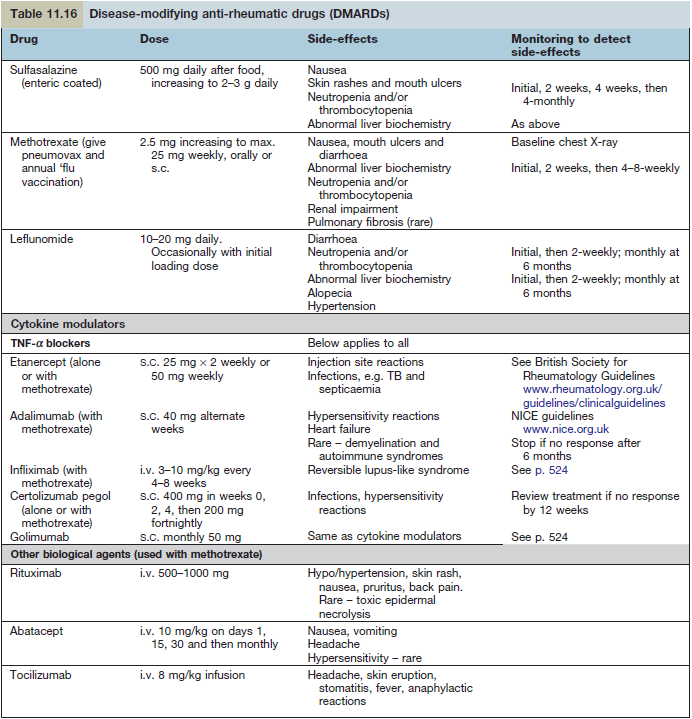
- DMARDS – first line treatment
- Sulfasalazine [500mg/ after meal 2g/day] – safe in preg, need to monitor blood (leukopenia/thrombocytopenia)
- Methotrexate [25mg/week] – gold standard, FBC/LFT monitored
- Leflunomide [20mg/day] – inhibit T cell expansion via inhibition of dihydroorotate dehydrogenase. Immunomodulation.
- Hydroxychloroquine – check macular function as retinopathy is irreversible.
- TNF blockers
- Etanercept [50mg/week], adalimumab, infliximab, certolizumab (Fab)
- Used with methotrexate to increase efficacy
- Others
- D-penicillamine, azathioprine, gold, ciclosporin, rituximab, tocilizumab (IL-6)