1. SAN RHYTHMS
Sinus arrhythmia
- Phasic alteration of the heart rate (HR) during respiration – sinus rate (SR) ↑ during inspiration and ↓during inspiration
- Consequence of normal parasympathetic nervous system (PNS) activity
Sinus bradycardia
- SR <60bpm may occur in healthy people at rest or athletes
- Pathological causes – MI, sick sinus syndrome, hypothyroidism, drugs (BB, digoxin), carotid sinus pressure
- IV atropine [0.6-1.2mg] for symptomatic patients
Sinus tachycardia
- SR >100bpm
- Due to ↑sympathetic NS activity – exercise, emotion, pregnancy
- Pathologic causes – anxiety, fever, anaemia, thyrotoxicosis, heart failure, drugs (B-agonists)
Sick sinus syndrome
- MC in elderly people
- Fibrosis, degenerative changes or ischemia of the sino-atrial node (SAN)
- CF – sinus bradycardia, sinoatrial block, tachycardia
- Pacemakers indicated for pts symptoms due to spontaneous bradycardia
2. ATRIAL TACHYARRHYTHMIAS
Atrial ectopic beats (extrasystoles, premature beats)
- Usually cause no symptoms. Sometimes a sensation of heaviness of the heart
- ECG – shows a premature but normal QRS
- If visible, the P wave has a different morphology because the atria activate from an abnormal site
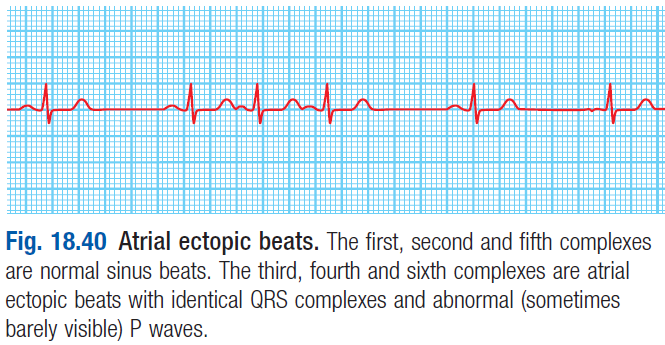
Tx rarely needed – BB if sx are troubling
- If visible, the P wave has a different morphology because the atria activate from an abnormal site
Atrial tachycardia
- May be due to ↑atrial Automaticity, Triggered activity or Re-entry
- ECG – narrow QRS complex (<0.12s) with abnormal P waves
- Treatment
- BB (which ↓automaticity) or class I or III antiarrhythmics
- Ablation – to target the ectopic site
Atrial flutter
- Characterised by a large re-entry circuit within the right atrium, circling around the tricuspid annulus
- Atrial rate is 300bpm (if every beat conducts [rare])
- Usually associated with AV block – 2:1 is MC
- Therefore every 2nd beat conducts – giving a ventricular rate of 150bpm
- ECG – saw toothed (flutter) waves
- Can be difficult to see flutter waves in 2:1 block as they are buried in the QRS complex
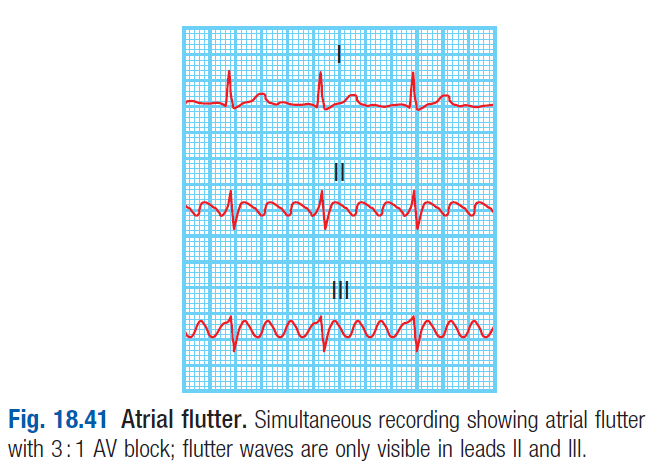
Carotid sinus massage slows the AV block and reveal the flutter waves
- Treatment
- DC cardioversion – to restore sinus rhythm
- Catheter ablation
- BB or amiodarone [200mg t.i.d] – to prevent recurrent episodes
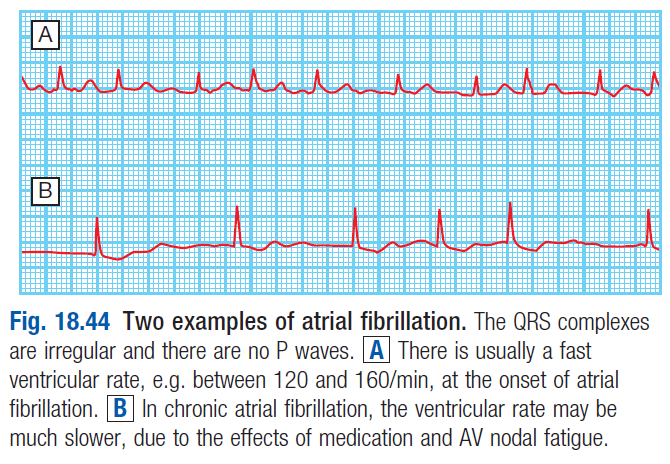 Atrial fibrillation (AF)
Atrial fibrillation (AF)
- Characterised by
- Accelerated automaticity
- And multiple interacting re-entry circuits looping around the atria
- Episodes of AF are initiated by rapid bursts of ectopic beats arising from conducting tissue in the pulmonary veins or diseased atrial tissue
- Then AF becomes sustained because of re-entrant conduction
- Re-entry is more likely to occur in enlarged atria e.g. in heart disease
- During episodes of AF the atria beat rapidly but uncoordinated and ineffectively
- So the ventricles are activated irregularly – results in Irregularly irregular pulse
- ECG – shows normal but irregular QRS. No p waves
- Oscillations of the baseline
- AF can be paroxysmal (intermittent episodes that self-terminate within 7 days), An Persistent/permanent
- Long term AF leads structural remodelling – atrial fibrosis and dilation
- Predisposes to further AF
- Causes of AF – CAD, valvular heart disease, HTN, hyperthyroidism, cardiomyopathy
 CF – palpitations, SOB, fatigue, chest pain
CF – palpitations, SOB, fatigue, chest pain
- Can precipitate or aggravate HF
- Associated with stroke and systemic embolism
Treatment
- Tx primary disorder
- Acute AF
- Control ventricular rate – see below
- Anticoagulation – warfarin
- Cardioversion – with DC shock or drugs (IV flecainide, propafenone)
- Chronic AF
- Rate control – digoxin, BB or NDP-CCB (verapamil/diltiazem)
- Rhythm control
- Patients with no heart disease – class Ia, Ic or III drugs
- Patients with HF/Left ventricular hypertrophy – amiodarone
- Patients with paroxysmal/early AF – LA ablation
- Anticoagulation
- Indicated in pts with AF related to rheumatic mitral stenosis or in patients with prosthetic heart valve
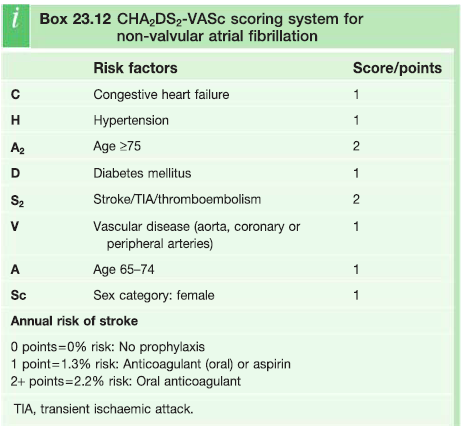
- In patients with non-valvular AF, CHA2DS2VASc system is used to determine need for anticoagulation
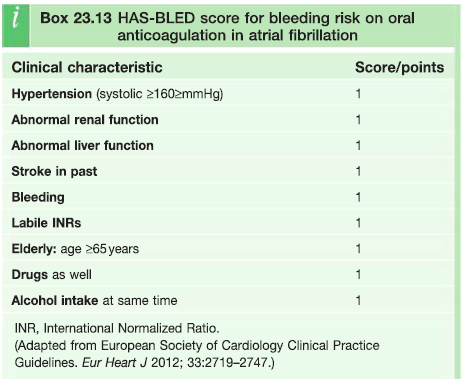
Prophylaxis against ischemic stroke with anticoagulation must be balanced against risk of haemorrhage using the HAS-BLED score- Warfarin – INR 2-3
- Direct thrombin inhibitor – dabigatran
- Direct factor Xa inhibitor – rivaroxaban
3. ATRIOVENTRICULAR JUNCTIONAL TACHYCARDIAS
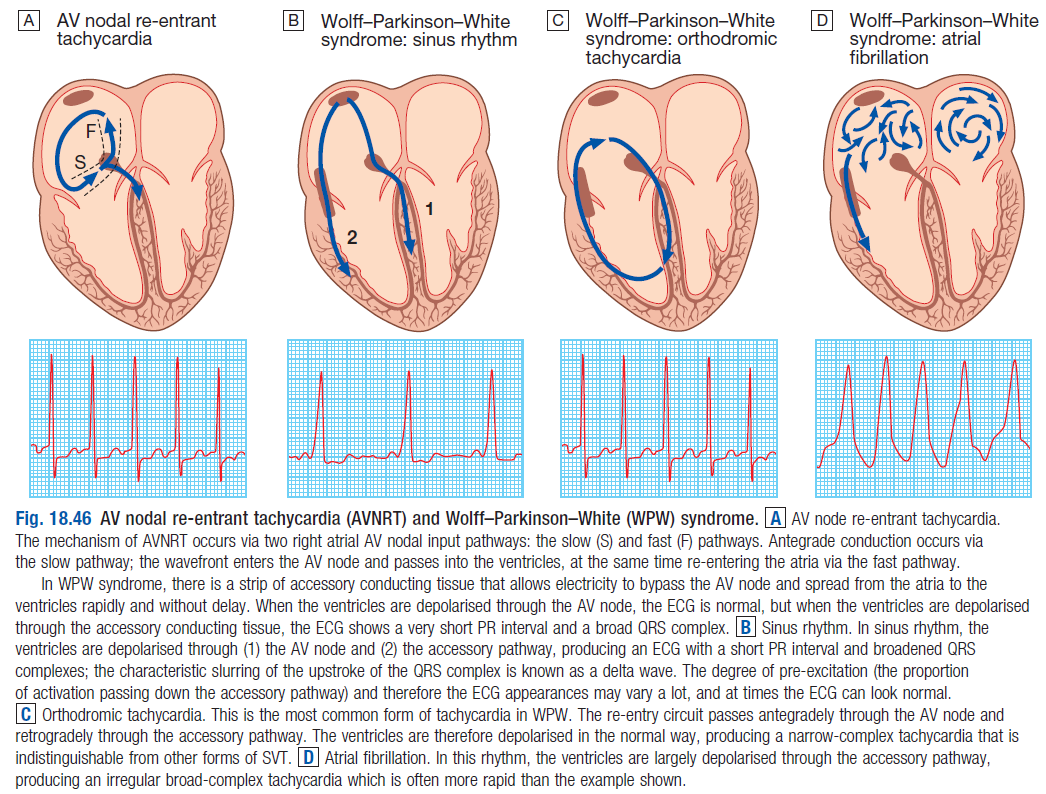
AV nodal re-entrant tachycardia (AVNRT)
- MC in women
- CF – rapid, forceful, regular heart beat
- Characterised by 2 different pathways in the AVN
- One with a short refractory period + slow conduction
- Other with long refractory period + fast conduction
- In normal sinus rhythm, the atrial impulse that depolarises the ventricles conducts through the fast pathway
- If an atrial premature beat occurs early when the fast pathway is still refractory, the slow pathway takes over in propagating the impulse to the ventricles
- It then travels back in a retrograde direction through the fast pathway, initiating the AVNRT
- ECG – normal QRS at 140-240bpm
- P waves either invisible or are immediately before or after the QRS because of simultaneous atrial and ventricle activation
AV re-entrant tachycardia (AVRT)
- This circuit comprises the AVN, His bundle, ventricle and an abnormal connection of myocardial fibres (accessory pathway [AP])
-
- Results from an incomplete separation of the atria and ventricles during fetal development
- MC accessory pathway is the Kent Bundles
- – in the septum
- Atrial activation occurs after ventricle activation – so P wave is seen between QRS and T wave
- Pathways that conduct in retrograde direction (ventricles→atria) are not seen on the ECG – concealed AP
- Bidirectional APs are seen on the ECG
- Conduction in sinus rhythm is mediated by both the AVN and the AP – this distorts the QRS
- Premature ventricular activation (pre-excitation) via the AP shortens the PR interval and produces a slurred deflection of the QRS – called the delta wave
- pts with a pre-excited ECG and palpitations have Wolff-Parkinson-White syndrome
Treatment
- DC cardioversion
- Carotid sinus massage or IV adenosine [6-12mg bolus] – for tachycardia
- Valsava manoeuvre