Etiology/Epidemiology
- 9x in women, 20-40y
- Hereditary, genetics, sex hormone status (premenopausal)
- Drugs – hydralazine, isoniazid, procainamide, penacillamine
- UV, EBV exposure
Pathology
- Ineffective removal of apoptotic self-antigens via Mθ. Resulting in B/T stimulation by APC in lymphoid follicles
- Complement and abnormal cytokine production (IL10/IFN alpha)
- Skin/kidneys – complement, IgG, neutrophil infiltration
- Haematoxylin bodies – inflammatory infiltrates (ANA and cell nuclei interaction)
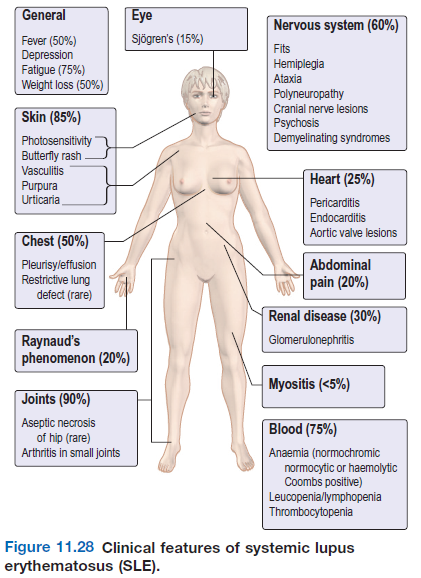
Clinical features
- General
- Fever, fatigue, arthralgia, weight loss, LAD
- Arthritis – like RA but erosions are rare. Avascular necrosis rare comp of CS tx
- Skin
- Butterfly rash , vascular lesions, purpura, urticaria, photosensitivity Ro +
- Alopecia may be permanent, raynauds phenomenon
- Discoid lupus – benign form only affects skin
- Lungs
- Pleurisy and effusions, pneumonitis/atelectasis bilateral
- Restrictive lung disease
- Heart/CV
- Pericarditis, myocarditis, libman sachs syndrome
- Raynauds, venous thrombosis, vasculitis – Anti-phospholipid syndrome
- Risk of MI and stroke
- Kidneys
- Lupus nephritis
- Renal vein thrombosis – antiphospholipid-antibodies
- CNS
- Depression, epilepsy, psychiatric disturbances, cerebrovascular disease
- Cerebral lesions may be due to immune complexes or vasculitis
- Eyes
- Vasculitis (cytoid bodies) – hard exudates and haemorrhages
- Episcleritis, optic neuritis, conjunctivitis.
- Secondary sjogren’s syndrome
- GIT
- Mouth ulcers common
- Mesenteric vasculitis and small bowel infarction
- Pregnancy
- Recurrent miscarriages – antiphospholipid-ab. Exacerbations happen post-partum
Diagnosis
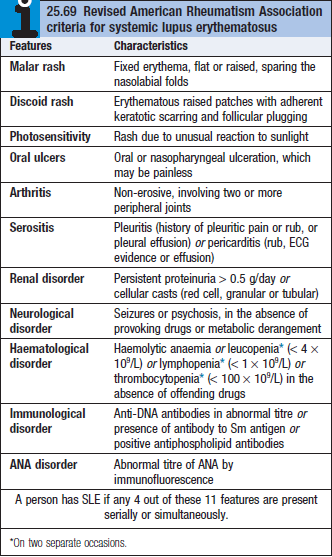
- 4/11 criteria must be fulfilled (see below)
- Blood (leukopenia), creatinine/urea (advanced renal disease), Auto-antibodies
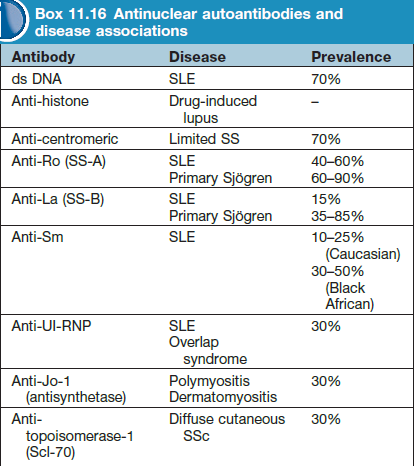
- Most common auto-ab – ANA, dsDNA, Ro, Sm, La
- C3 and c4 complement low in active disease
- CT/MRI – brain lesions – white matter
Treatment
- Single I.M long acting CS (5-20/day)
- Symptomatic tx, topical CS for skin
- Immunosuppressive drugs – mycophenolate mofetil , cyclophosphamide, azathioprine
- In preg – stop mycophenolate. Hydroxychloroquine (200-400), azathioprine, low dose CS are safe
- Life threatening – pulse methylprednisolone (10mg/kg) + cyclophosphamide (15mg/kg)