1. BENIGN LIVER LESIONS
- Benign liver lesions are more common than malignant tumours
Cyst
- Most common liver lesion
- Congenital Cysts
- More common in females
- Thin walled, homogenous, fluid-filled structure
- Cyst is lined by cuboidal epithelium – secretes a clear fluid
- Usually asymptomatic, unless they are very large
- Acquired cysts – secondary to trauma, infection or neoplasm
Hemangioma
- Consist of large endothelial-lined vascular spaces
- Contain fibrous tissue and small blood vessels that eventually grow
- They are congenital vascular lesions
- Can be small (<1cm) or giant (10-25cm)
- Most discovered incidentally
- Large lesions may compress adjacent structure and cause symptoms
- Complications – bleeding, thrombosis, DIC, infection
- Investigations – CT, MRI
- Treatment – enucleation/hepatic resection/radiation in adults
Adenoma
- Benign, solid neoplasms
- Can be single or multiple (>10 is called adenomatosis)
- Most common in premenopausal women over 30 years old – use of OCP is a risk factor
- Histology
- Lack bile duct glands and Kuppfer cells
- Don’t have true lobules
- Hepatocytes are vacuolated due to glycogen deposition
- Investigations
- CT – shows sharp borders
- MRI – with gadoxetate (liver specific MRI contrast)
- Complications
- Risk of spontaneous rupture with intraperitoneal bleeding
- Malignant transformation into hepatocellular carcinoma
- Treatment – hepatic resection
Focal nodular hyperplasia
- Benign lesion of liver thought to be a hyperplastic response to an anomalous artery
- Most common in premenopausal women
- Histology – contains Kuppfer cells and hepatocytes
- Investigations
- CT – shows well circumscribed lesion with central scar
- Unlike adenomas, they do not rupture spontaneously and have little risk of malignant transformation
- Treatment – observation and periodic checks
2. HEPATOCELLULAR CARCINOMA
Epidemiology
- Most common primary malignant neoplasm of liver
- Most prevalent in areas with high incidence of HBV
- Common in Africa and China
- Most common in men 50-60 years old
Etiology
- HBV, HCV, cirrhosis, non-alcoholic fatty liver disease
- Aflatoxin (product of fungus aspergillus)
- Hepatic adenoma
Pathology
- 3 distinct gross patterns
- Hanging type – connects to normal liver via vascular stalk (very resectable)
- Pushing – well demarcated with fibrous capsule. Displaces normal vasculature (resectable)
- Infiltrative type – invades vascular structures (difficult to resect)
- Begins as a single tumour but can lead to multiple lesions due to invasion and metastasis
Clinical features
- Non-specific symptoms – fatigue, fever, weight loss, lethargy
- Right upper quadrant pain – uncommon, but suggestive of HCC in a cirrhotic patient
- Enlarged, tender liver
- Jaundice
- Ascites
Investigations
- AFP >500ng/ml (>100 IU)
- LFTs
- US abdomen
- CT – shows size, extent, location, vascularity, portal vein invasion and nodal status
- CT angiography
- Biopsy –definitive
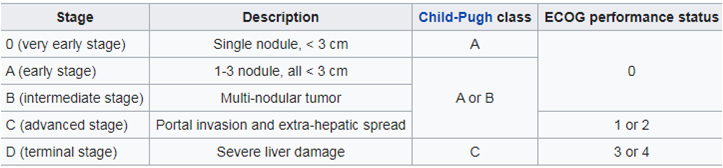
Staging
Barcelona Clinic Liver Cancer (BCLC) Classification
Treatment
- Curative – partial hepatectomy, liver transplant
- Palliative – embolisation, thermal/radiofrequency ablation
- Chemo has limited benefits
3. GALLBLADDER CANCER
- Aggressive malignant disease – poor prognosis
- Usually presents at a late stage
Epidemiology
- Most common in 60-70 year olds, especially in females
- Highest incidence in India and Pakistan
Etiology
- >90% of patients have associated Cholelithiasis
- Risk factors – obesity, female sex, primary sclerosing cholangitis
Pathology
- Adenocarcinoma is the most common type
- Other types – squamous cell carcinoma, adenosquamous carcinoma, carcinoid tumour
- Gradual progression from dysplasia → carcinoma in situ → invasive carcinoma
- Mainly found in fundus/body of the gallbladder
Spread
- Direct spread – to liver (segment IV and V), bile duct, duodenum, colon kidney
- Lymphatic – lymph node of Lund, peripancreatic and periduodenal nodes
- Haematogenous – liver, lungs, bones
Clinical features
- Most are asymptomatic until advanced disease
- Weight loss, jaundice, abdominal mass
- Chronic epigastric pain
- Early satiety
- Courvoisier’s law – presence of a palpably enlarged, non-tender gallbladder accompanied by mild jaundice is unlikely to be gallstones and is presumed to be due to malignancy of the gallbladder or pancreas
Investigations
- US – shows irregular shaped and asymmetrical thickened gallbladder wall
- CT for staging
- MRCP
- CA 19-9
Treatment
- Surgery – only curative option
- Cholecystectomy with resection of liver segment IV + V
- Clear all pericholedochal lymph nodes
- Palliative procedure – endoscopic/percutaneous stents to treat jaundice
4. CHOLANGIOCARCINOMA
- Rare tumour arising from biliary epithelium – can occur anywhere in biliary tree
- Most commonly localised at hepatic duct bifurcation
- Usually presents when disease is advanced
- Age of presentation – >50 years old
Etiology
- Associated with
- Caroli’s disease – inherited, cystic dilation of intrahepatic bile ducts
- Clonorchiasis – Chinese liver fluke parasite
- Risk factor – primary sclerosing cholangitis, choledocal cyst, HBV/HCV
Pathology
- 95% are adenocarcinomas
- Locations
- Intrahepatic
- Perihilar/bifurcation – AKA Klatskin tumours (further classified in the Bismuth classification – see below)
- Distal
Classification – Bismuth Classification
- I – limited to the common hepatic duct, below the confluence of the right and left hepatic ducts
- II – involves the confluence of the right and left hepatic duct
- III – (a) type II and extends into right hepatic duct (b) type II and extends into the left hepatic duct
- IV – extends to the bifurcations of both right and left hepatic ducts
Clinical features
- Klatskin tumour is more likely to present with obstructive jaundice
- Intrahepatic tumour is more likely to present with a liver mass
- Painless jaundice, pruritis
- Right upper quadrant pain
- Weight loss, anorexia, fatigue
Investigations
- Blood – ↑ALP, ↑GGT,↑CA 19-9
- MRCP/ERCP
- US, CT
Treatment
- Surgical excision – only curative treatment
- For intrahepatic or Klatskin tumours
- Partial hepatectomy, cholecystectomy
- For distal bile duct tumours – Whipple’s (pancreaticoduodenectomy)
- Pancreaticojejunostomy, gastrojejunostomy, choledojejunostomy
- Palliative treatment
- Roux-en-Y hepaticojejunostomy
- Insertion of stents
