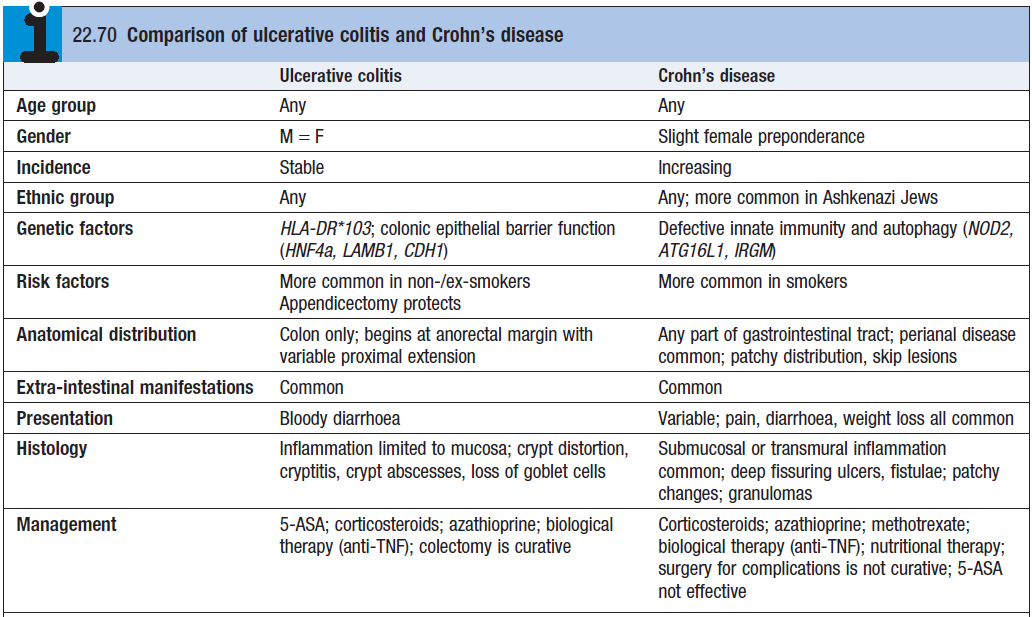
- Relapsing and remitting inflammatory bowel disease (IBD) of the colonic mucosa.
- May just affect the rectum (proctitis); extend to involve part of the colon (left-sided colitis); or the entire colon (pancolitis)
Epidemiology
- MC in developed countries – in Caucasians, Ashkenazi Jews
- All ages susceptible but MC in pts <30yr
- MC in non smokers
Etiology
- Unknown – environmental and genetic components – HLA-B27 association
- Family history of IBD is risk
Pathology
- UC develops as a result of an environmental trigger in a genetically susceptible person
- Starts in the rectum and spreads proximally – rectum is involved in all circumstances
- UC is a diffuse inflam disease, primarily affecting the mucosa + submucosa
- Only in severe cases are the deeper layers of the intestinal wall affected
- Multiple minute ulcers
- Chronic cases – inflammatory polyps (pseudopolyps)
- Severe fulminant colitis – section of the colon (MC transverse colon) becomes acutely dilated with risk of perforation (toxic megacolon)
- Histology – ↑inflam cells in lamina propria (TNF-a, IL-12, IL-18). Walls of the crypts are infiltrated by inflam cells (crypt abscess)
- Depletion of goblet cell mucin. With time precancerous changes can develop
Clinical features
- Episodic or chronic diarrhoea – with or without blood + mucus
- Crampy abdominal discomfort
- Relapsing and remitting course
- Urgency/tenesmus
- Systemic features – fever, malaise, anorexia, WL
- Extra-intestinal signs
- Clubbing, aphthous oral ulcers, erythema nodosum, pyoderma gangrenosum, conjunctivitis, arthritis
- Emotional stress, infections, gastroenteritis, antibiotics, NSAIDs can provoke a relapse
Investigations
- Blood – FBC, ESR, CRP, U+E, blood culture,
- Stool – to exclude Campylobacter, C.difficile, Salmonella, Shigella, E.coli
- Calprotectin – accurate marker for GIT inflammation
- AXR – no faecal shadows, mucosal thickening, colonic dilation
- Erect CXR – perforation
- Barium enema – never perform during acute attacks
- Colonoscopy shows disease extent and allows biopsy – look for inflammatory infiltrate, goblet cell depletion, glandular distortion, crypt abscesses
- Backwash ileitis
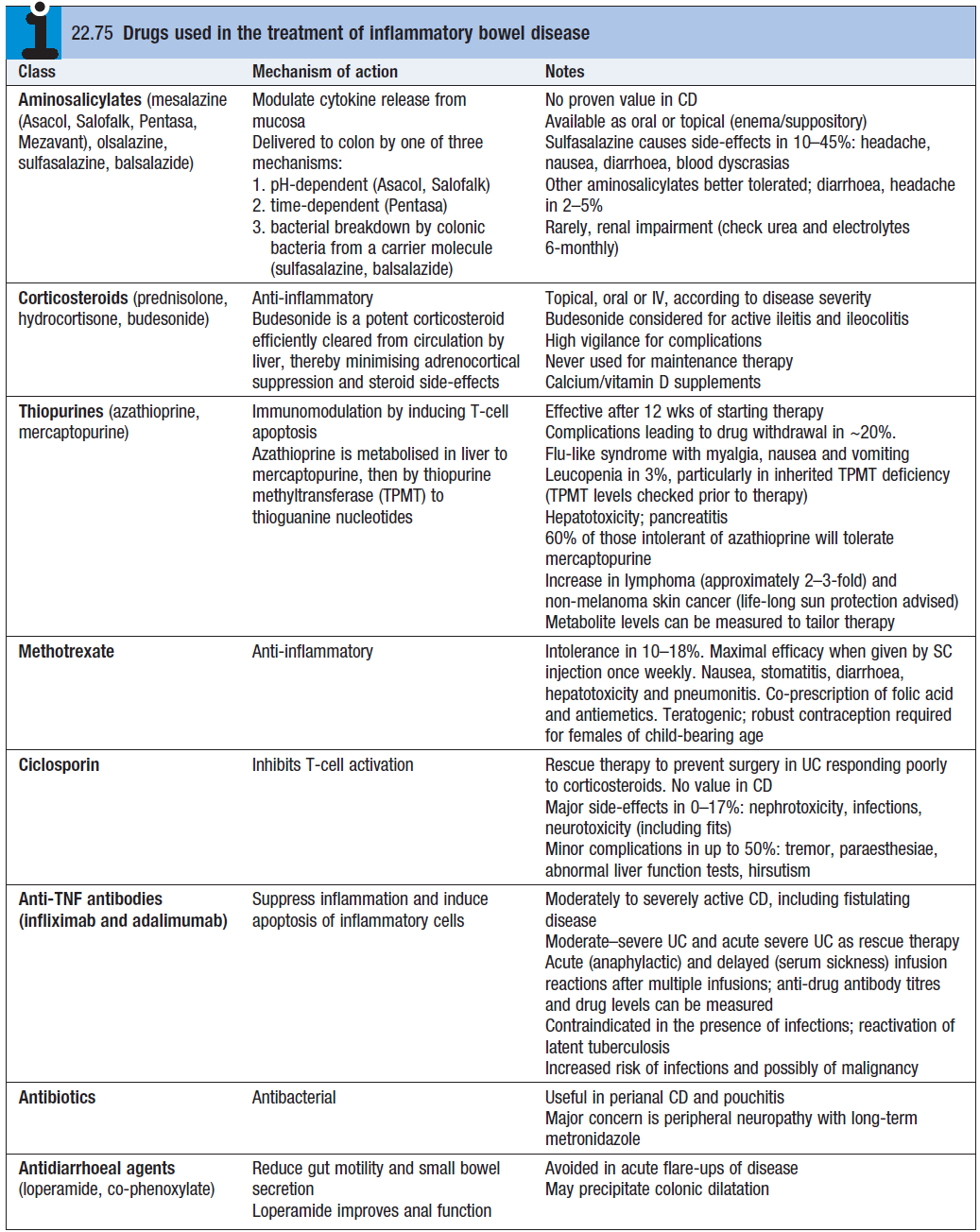
Treatment
- Sulfasalazine or mesalamine (5-ASA) – first line. [2-4g/day]
- Remission induction. Inhibits PG E1+E2 to reduce inflam
- Oral presnisolone – for refractory cases
- [40mg daily, tapered by 5mg/week over an 8 week period]
- Venous thrombus prophylaxis
- Heparin [5K/12hrs]
- Fondaparinux [2.5mg/day]
- Severe cases
- Thrombo prophylaxis, I.V hydration, nil-by-mouth, hydrocortisone [100mg/6hrs I.V]
- Rescue therapy – infliximab, cyclosporin
Surgery – often curative (unlike CD),
- Involves total colectomy with ileo-anal anastomosis and a pouch (acts as a reservoir for stool)
- Indications for surgery
- Severe, debilitating, refractive disease unresponsive to medical therapy
- Toxic megacolon (risk of perforation), obstruction due to stricture, severe haemorrhage, perforation
- Fulminant exacerbation that doesn’t respond to steroids
- Evidence of increased risk of colon cancer
- Growth failure or failure to thrive
Complications
- Perforation and bleeding
- Toxic megacolon
- Venous thrombosis
- Colonic cancer – risk is 15% with pancolitis for 20 years
- Strictures – benign and malignant
- Cholangiocarcinoma – half of all bile duct cancers assoc with UC