1. MYELOFIBROSIS (MF)
Epidemiology
- MC in older people
- Assoc with exposure to benzene and ionizing radiation
- Secondary MF can develop from other MPDs (PV or ET)
Pathophysiology
- Characterised by a leukoerythroblastic reaction in blood (nucleated RBCs & immature granulocytes), splenomegaly and BM fibrosis .
- Clonal disease of hematopoietic stem cells
- Malignant megakaryocytes and monocytes drive fibroblasts to produce excess collagen
- Cytokines involved are – TGF-β, PDGF
- Extramedullary hematopoiesis in spleen causes splenomegaly
Clinical features
- Fatigue, cachexia, weight loss, LGF, night sweats
- Marked splenomegaly – early satiety, LUQ discomfort
- Physical exam – spleen can extend to pelvic brim
- Mild hepatomegaly
Diagnosis
- Anaemia
- Cytopenias
- WCC – mostly ↑ due to granulocytosis (but can be ↓)
- Platelets – mostly ↑
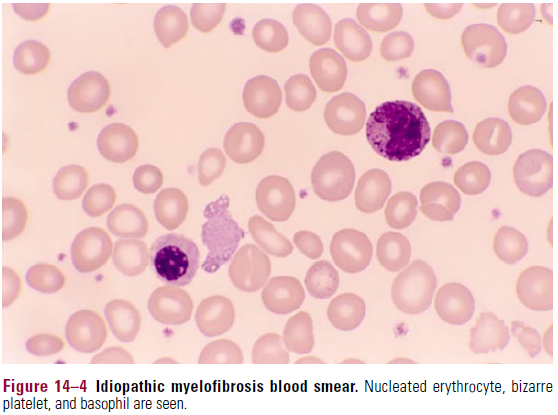
- Blood smear – most striking (see pic)
- Teardrop RBCs , nucleated RBCs, immature granulocyte precursors, giant platelets

- ↑LDH, UA, LAP
- Bone marrow
- Dry tap – cannot be aspirated
- Can have near total replacement by collagen (reticulin type)
- ↑megakaryocytes
- Cytogenetics
- JAK-2 mutation – in 50% of cases
- If XR mut – osteomyelosclerosis
Disease course
- Younger pts and those without anemia have longer survival time
- MCC of death – haemorrhage, infection, heart failure
- Can progress to AML
- Splenomegaly – can cause portal HTN, and pts can develop hematmesis from varices
- Patients can develop extramedullary hematopoiesis (EMH) in other locations – e.g. in LNs, skin, pleural cavity, CNS
Treatment
- Largely palliative
- Transfusions
- Corticosteroids
- Hydroxyurea (first choice)
- Splenectomy not indicated as EMH can shift to liver – patients can die from liver dysfunction
- BMT – in younger pts
