Chronic Heart Failure – etiology, pathogenesis, circulatory disturbances, classification, clinical features, diagnosis, treatment
- Clinical syndrome that develops when the heart cannot maintain adequate output, or can do so only at the expense of elevated ventricular filling pressures
Etiology
- Ischemic heart disease (IHD) – myocardial infarction (MI)
- Dilated cardiomyopathy
- Hypertension (MC elderly hypertensive)
- Valvular heart disease
- Congenital heart disease
- Right heart failure (PHTN, PE, COPD)
Pathophysiology
- Cardiac output is determined by
- Preload – volume and pressure of blood in the ventricles at the end of diastole
- Afterload – pressure required to open the aortic valve
- Myocardial contractility
- Impairment of ventricular myocardial function is main abnormality – leads to a fall in cardiac output (CO)
- Can be due to impaired systolic contraction and/or impaired diastolic relaxation
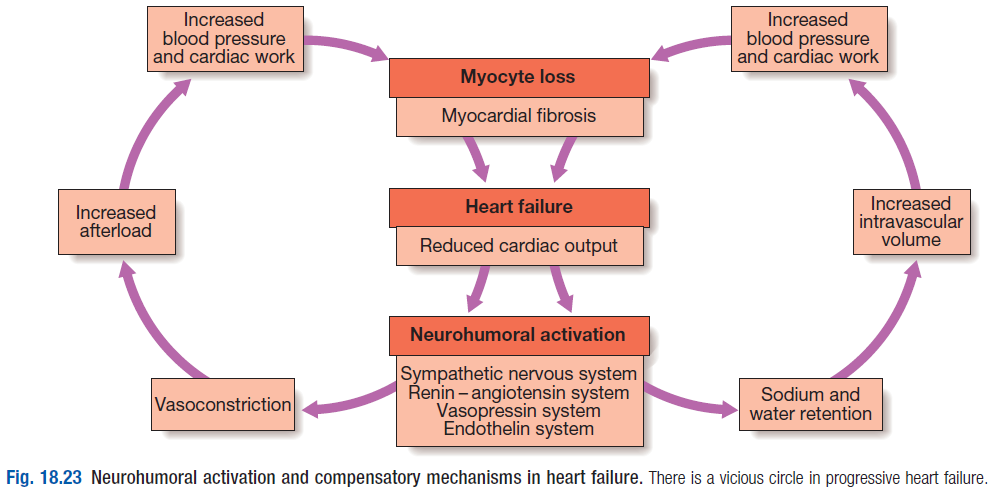
- This activates counter-regulatory neurohormonal mechanisms – leads to ↑preload and afterload
- Reduced CO and therefore renal perfusion stimulates activation of Renin – angiotensin – aldosterone system (RAAS)
- Stimulation of RAAS → vasoconstriction; Na + water retention; SNS activation
- Mediated by angiotensin II – which is a potent constrictor of arterioles in kidney and systemic circulation
- ANS – SNS activity initially ↑contractility (inotropy) and heart rate (HR) (chronotrophy) – sustains CO
- But prolonged stimulation causes negative effects – cardiomyocyte apoptosis, hypertrophy, necrosis
- SNS also causes peripheral vasoconstriction and arrhythmias
- Aldosterone and ADH (vasopressin) release promotes retention of Na and water
- Natriuretic peptides (BNP/ANP) released from the atria in response to atrial stretch antagonise the fluid-conserving effect of aldosterone
Remodelling
- LV remodelling is a process of progressive alteration of ventricular size, shape and function due to the influence of mechanical, neurohormonal and genetic factors
- Seen in MI, cardiomyopathy, HTN
- Hypertrophy, loss of myocytes, interstitial fibrosis
Types of heart failure
Left, Right and Biventricular heart failure
- Left heart failure
- Reduction of LV output and increase in left arterial pressure (LAP) and pulmonary venous pressure
- An acute rise in LAP causes pulmonary congestion and oedema
- A gradual rise in LAP leads to reflex pulmonary vasoconstriction – protect pt from pulm congestion, but in turn leads to PHTN, which can then impair RV function
- Right heart failure (RHF)
- Reduction in RV output and increase in LAP and systemic venous pressure
- Causes of isolated RHF – corpulmonale, PE, pulmonary valve stenosis
- Biventricular heart failure
- Diseases such as ischemic heart disease/dilated CMO affect both ventricles
Systolic dysfunction –HFrEF (reduced ejection fraction)
- HF due to impaired myocardial contraction
- MC in IHD, valvular heart disease
Diastolic dysfunction – HfpEF (preserved ejection fraction)
- Increased stiffness and decreased compliance of LV – leads to impaired diastolic ventricular filling and ↓CO
- MC in elderly hypertensive pts
High output failure
- Excessively high CO due to arteriovenous shunt, Beri-beri , anaemia, thyrotoxicosis
Acute and chronic HF
- Acute HF (decompensated) – can develop suddenly. Presents overtly (PCWP >16mmHg = poor prognosis)
- E.g. HF in MI
- Chronic HF (compensated) – adaptive, compensatory mechanisms prevent the development of overt HF
- E.g. in valvular diseases
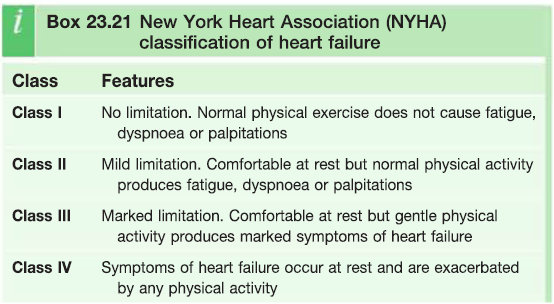
Clinical features
- Chronic HF pts have a relapsing and remitting course – periods of stability and then periods of decompensation
- Fatigue, restlessness, poor effort tolerance, cold peripheries – due to ↓CO
- Oliguria, uraemia – due to poor renal perfusion
- Dyspnoea, Pulmonaryoedema – LHF
- High JVP, hepatic congestion, peripheral oedema – RHF
- Cardiac cachexia – GI congestion causes impaired absorption
Complications
- Renal failure, hypo/hyperkalaemia, hyponatremia, impaired liver function, thromboembolism, arrhythmias
Diagnosis
- Blood test – FBC, U+E, LFT, BNP, thyroid function
- Monitor – FLUID, FUNCTION, RHYTHM
- CXR – cardiomegaly, pulmonary congestion, Kerley B lines
- ECG
- ECHO – chamber size, systolic/diastolic function, valvularabnormalities, cardiomyopathies. Stress ECHO w/ dobutamine
- Cardiac MRI – cardiac structure, function and viability
- Cardiac catheterisation – dx of IHD and measurement of pulmonary artery pressure, LAP (wedge)
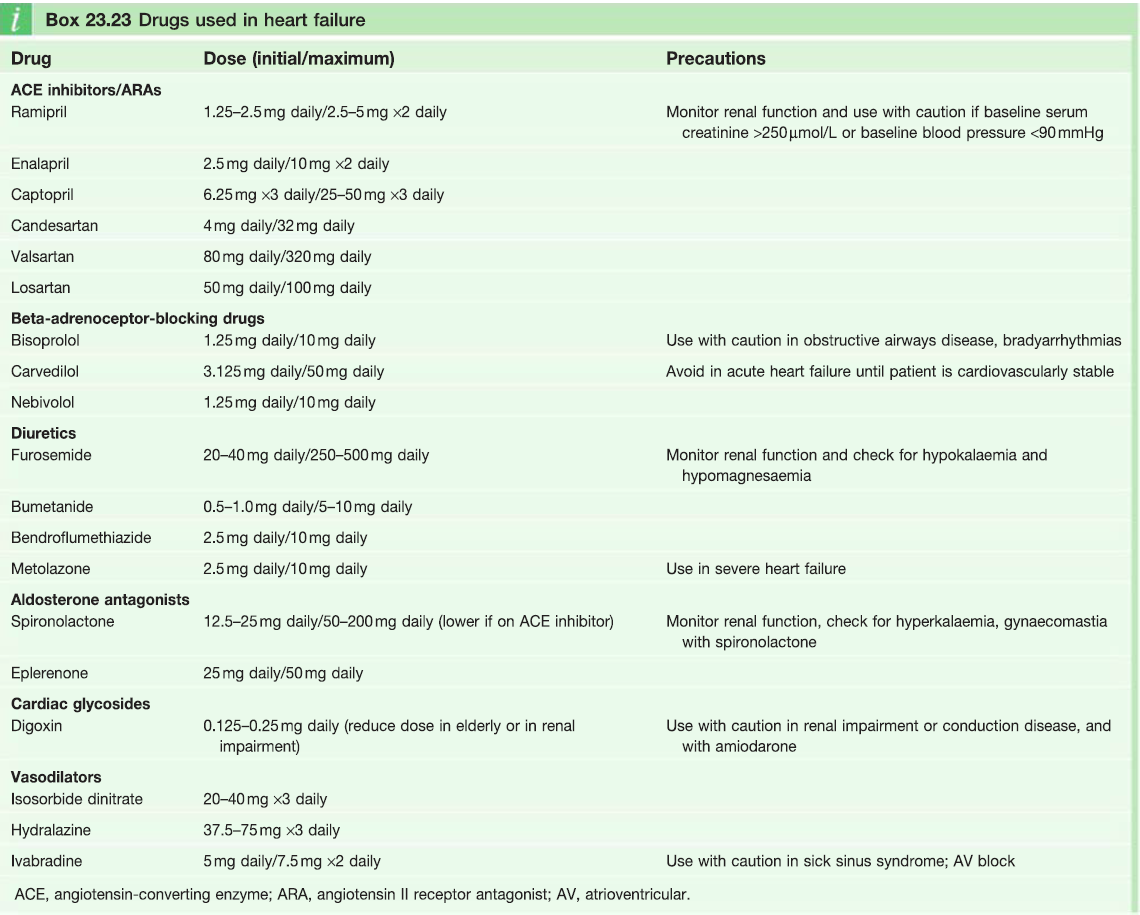
Treatment
Drug therapy –aim to increase contractility, optimise preload and decrease afterload
- Diuretics – ↓preload, improves pulmonary and systemic venous congestion
- Loop + thiazides can be combined for resistant oedema
- Mineral corticoid receptor antagonist – can cause hyperkalemia when combined with ACEi
- ACE inhibitors – interrupts vicious circle of neurohormonal activation (prevents conversion of AT I → AT II)
- Prevents peripheral vasoconstriction, SNS activity, Na + salt retention
- ARBs – block the action of AT II
- Better tolerated than ACEi
- Vasodilators
- Nitrates (venodilators) – reduce preload
- Hydralazine (arterial dilators) – reduce afterload
- Beta blockers – counteract effects of ↑SNS activity, reduces risk of arrhythmias and sudden death
- Contra-indicated in acute HF due to negative inotropic effects
- Ivabradine – acts on If inward current on the SAN, results in ↓HR
- Digoxin – rate control
ICDs + resynchronisation
- Can reverse the process of ventricular remodelling and improve LV function
Heart transplant
- Treatment of choice for young pts with severe HF
- Complications – rejection, infection