Etiology
- Congenital – bicuspid AV
- Acquired
- Rheumatic disease
- Infective endocarditis
- Trauma
- Aortic dilation – Marfan’s, aneurysm, dissection
- Acute causes – endocarditis, dissecting aorta rheumatic fever
- Chronic causes – rheumatic heart disease, bicuspid AV, syphilis, osteogensis imperfecta, marfan, SLE, arteritis
Pathogenesis
- AR is the reflux of blood from the aorta into the LV during diastole
- LV dilates and hypertrophies to compensate for the regurgitation and to maintain CO
- The SV of the LV can eventually be doubled
- Major arteries become visibly pulsatile
- Because of the decreased blood in the aorta during diastole, diastolic BP falls – coronary perfusion decreases
- As disease progresses, LVDP increases and breathlessness develops
Clinical features
- Significant symptoms occur late. The early symptoms are
- Palpitations, breathlessness
- Angina
- Collapsing pulse
- ↑pulse pressure
- Austin Flint murmur – soft, low pitched, rumbling mid-diastolic (indicates severe AR)
Signs – indicate hyperdynamic circulation
- Quincke’s sign – capillary pulsation in nail beds
- de Musset’s sign – head nodding with each heart beat
- Duroziez’s sign (severe AR) – murmur heard when femoral artery auscultated
- Pistol shot femorals – sharp bang heard with each heart beat upon auscultation of femoral artery
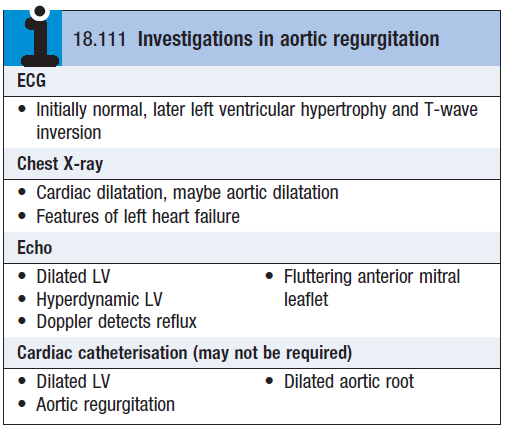
Investigations
Treatment
- Treat underlying conditions e.g. endocarditis
- Follow up asymptomatic patients with yearly ECHO for evidence of increasing ventricular size
- Control SBP – CCB (nifedipine)/ACEi
- Aortic valve replacement (±CABG/aortic root replacement) – if patient is symptomatic
